Optimal pediatric timing for kidney transplant in lupus nephritis: a survey study
Monika Sullivan1, Aesha Maniar1, Abanti Chaudhuri 1, Brian Stotter2, Scott Wenderfer3.
1Pediatric Nephrology, Stanford University, Palo Alto, CA, United States; 2Pediatric Nephrology, Washington University School of Medicine, St. Louis, MO, United States; 3Pediatric Nephrology, University of British Columbia, Vancouver, BC, Canada
Introduction: There is no evidence to guide optimal timing of kidney transplant in children with lupus nephritis after achieving lupus disease quiescence. These patients are less likely to receive a transplant within one year of starting dialysis compared to patients with other causes of end stage kidney disease. Understanding how pediatric nephrologists define lupus disease quiescence is important in determining transplant timing.
Methods: This is a survey study of pediatric nephrologists to determine practice patterns in managing children with lupus nephritis who require kidney transplant. The survey was distributed to members of the Pediatric Nephrology Research Consortium (PNRC), a voluntary network of academic pediatric nephrology practices across the United States. Survey questions pertained to pre- and post- transplant lupus management, lupus nephritis disease monitoring, defining disease quiescence, transplant timing, and psychosocial barriers to transplant. Data was collected in REDCap and analysis was performed in R Studio.
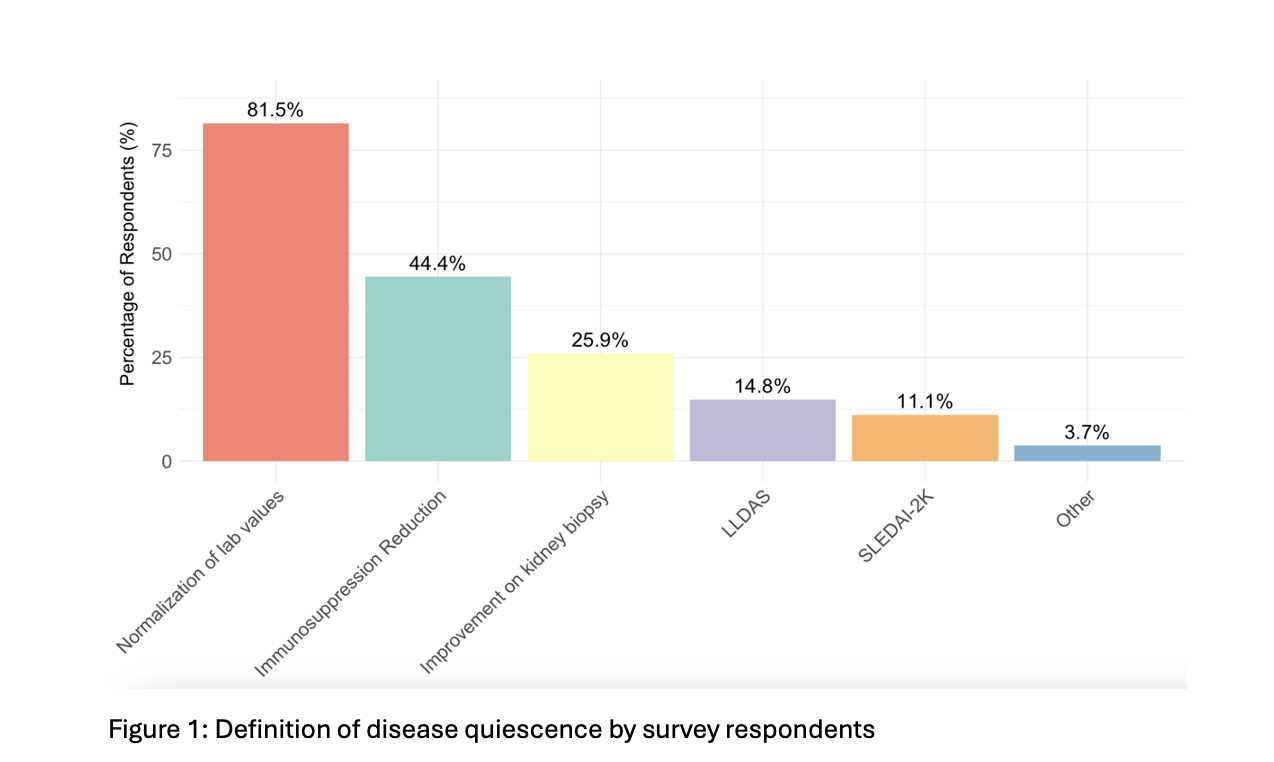
Results: To define lupus disease quiescence, most centers (81.5%) rely on the normalization of laboratory values and urine studies. Other commonly used criteria include a reduction in immunosuppression needs, such as steroid tapering (44.4%), and improvement or resolution of histologic disease activity on kidney biopsy (25.9%). Fewer centers use formal indices, such as the Lupus Low Disease Activity State (LLDAS) (14.8%) or the SLEDAI-2K (Systemic Lupus Erythematosus Disease Activity Index) (11.1%).
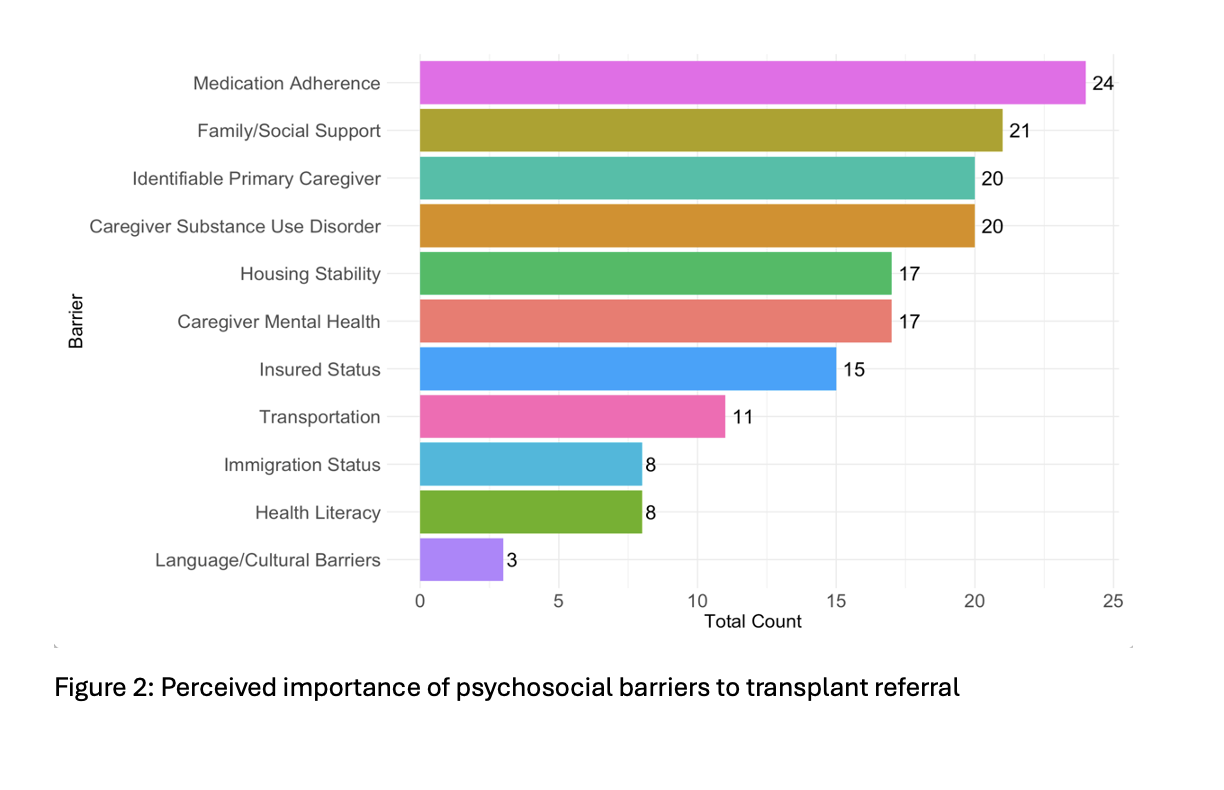
Among respondents who selected normalization of lab values, the most cited labs were complement levels (74.1%), proteinuria (66.7%), anti-dsDNA antibody (59.3%), and ESR (51.9%), with platelet and white blood cell counts less commonly used (33.3% each). Many centers (63.0%, n=17) prefer to see lupus disease quiescence for 6–12 months prior to activating a patient for transplant while a smaller proportion prefer 3–6 months (22.2%, n=6) or 0–3 months (7.4%, n=2) and few centers require quiescence for more than 12 months (3.7%, n=1). Pre-emptive kidney transplantation for lupus nephritis patients is performed or considered by 66.7% (n=18) of institutions, while 29.6% (n=8) reported not considering this approach. When asked about perceived importance of various psychosocial and socioeconomic barriers to transplant referral for patients with lupus nephritis, medication adherence was ranked the highest, followed by family/social support, identifiable primary caregiver, and caregiver substance use disorder.
Conclusion: The majority of pediatric nephrologists define lupus disease quiescence based on normalization or improvement of lab values rather than disease activity scoring tools. Most centers currently wait for 6-12 months of disease quiescence before transplant activation. Additional studies are necessary to determine the impact of wait time prior to kidney transplant on transplant outcomes in lupus nephritis patients.
[1] Immunosuppression
[2] Transplant timing
[3] Psychosocial barriers