Alternative, low-cost monitoring of CD3 cell depletion following anti-thymocyte globulin Induction in pediatric renal transplant recipients
Samantha Krieger1, Ruby Patel1, Paul Grimm1, Abanti Chaudhuri1.
1Pediatric Nephrology, Stanford University, Palo Alto, CA, United States
Background: Anti-Thymocyte Globulin (ATG), a polyclonal globulin, is an effective induction therapy for prevention of acute rejection in solid organ transplantation by targeting immunocompetent lymphocytes. ATG therapy carries significant risks of under - or overimmunosuppression leading to toxicity. Monitoring is crucial and aims for an absolute CD3 count <50 cells/mm³, indicating a 90–95% depletion of pretransplant T cells in the bloodstream. Flow cytometry tests for this measurement are expensive ($230/test), in contrast to the more affordable complete blood count (CBC) ($5/test). It has been proposed that the absolute lymphocyte count (ALC) obtained from the CBC could be utilized as a surrogate for the CD3 count to monitor immunosuppression effectiveness with ATG.
Methods: A retrospective analysis was conducted on 333 pediatric renal transplant recipients from a single center, stratified by CD3 count (<50 vs. >50) from 1/1/2014 to 10/1/2024. Data were analyzed for associations between ALC and CD3 counts, identifying threshold values with predictive significance. Patients were excluded if they received multiple transplants or had missing ALC counts.
Results: Our data had a natural division around the ALC of 200 K/µL (Fig 1). Among patients with ALC <200 (n=185) 91% had a CD3 count <50. Only 5.1% of patients had an ALC <200 but a CD3 count >50, and the majority of these cases had CD3 values near the threshold. Conversely, among patients with ALC >200 (n=148), 60% had a CD3 count >50, with 44% of those exceeding 100, indicating a potential need for immunosuppression adjustment. However, 41% of patients with ALC >200 still had CD3 <50, suggesting that ALC >200 is not an absolute determinant for further testing.
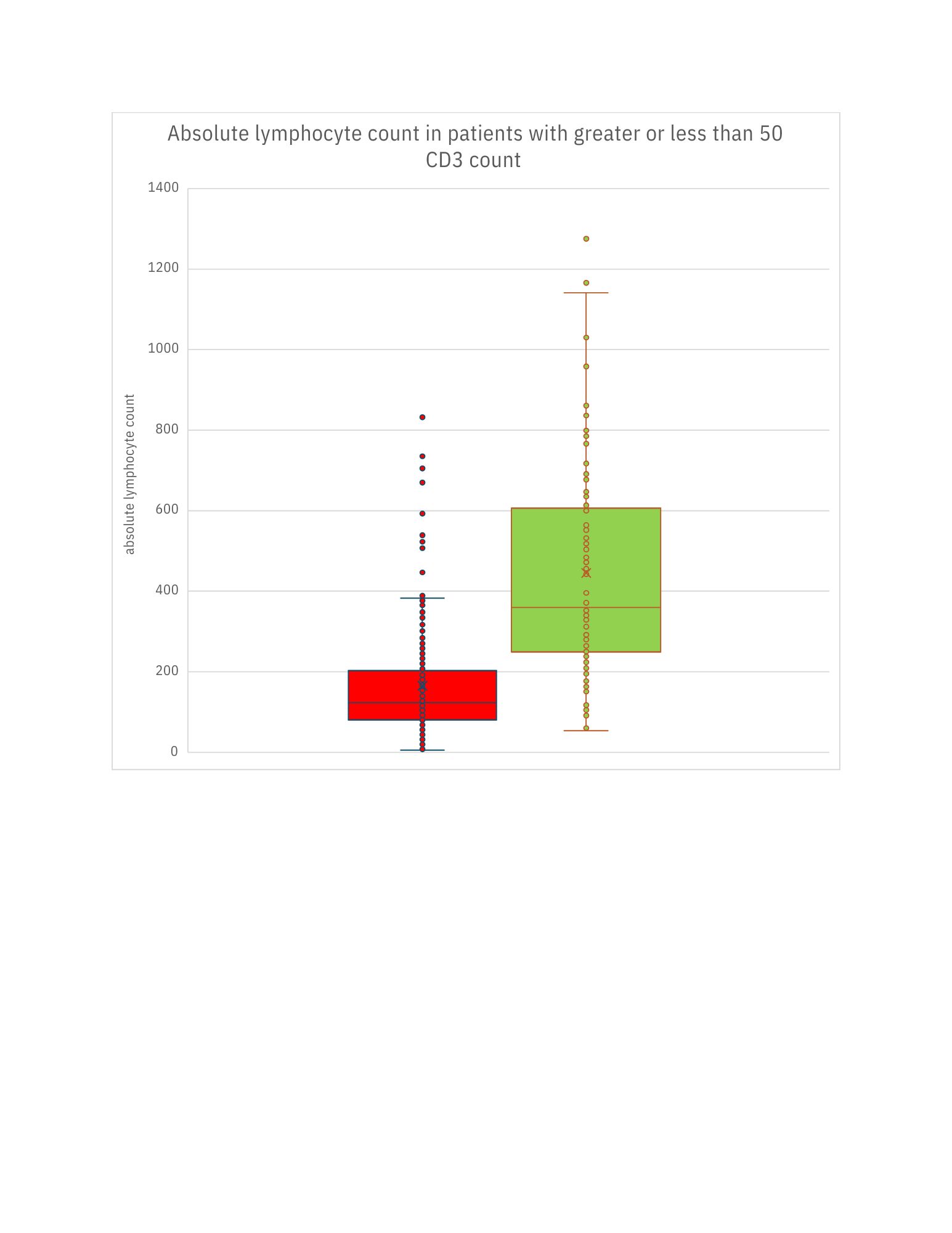
Conclusions: Our findings suggest that an ALC of 200 K/µL or below correlates with CD3 count of less than 50 cells/mm³ in majority of cases, leading us to believe that ALC can serve as a screening tool to guide the necessity of flow cytometry testing. We propose that If ALC <200, CD3 testing may be unnecessary. If ALC >200, flow cytometry should be considered, particularly in high-risk patients, while low-risk cases may be evaluated based on clinical context. Implementing this strategy could optimize resource utilization in post-transplant monitoring.
We are now testing our hypothesis by analyzing patient outcomes stratified by ALC examining the likelihood of acute cellular and antibody mediated rejection, viral infections, allograft function and graft loss.
[1] Absolute Lymphocyte Count
[2] Kidney Transplant
[3] CD3 Count