Prevalence and risk factors for pseudotumor cerebri syndrome in pediatric kidney transplant patients
Jonathan D Savant1, Samantha Najmola1, Yinxi Yu2, Gui-shuang Ying2, Grant T Liu3, Sonya Lopez1, Lauren Galea1, Bernarda Viteri1, Robert A Avery3, Sandra Amaral1.
1Division of Nephrology, Children's Hospital of Philadelphia, Philadelphia, PA, United States; 2Center for Preventive Ophthalmology and Biostatistics, Department of Ophthalmology, University of Pennsylvania, Philadelphia, PA, United States; 3Division of Ophthalmology, Children's Hospital of Philadelphia, Philadelphia, PA, United States
Background: Pseudotumor cerebri syndrome (PTCS) is rare, occurring in estimated 0.7 per 100,000 children, but can result in severe visual loss if unrecognized and untreated. The etiology of PTCS remains uncertain. Kidney disease has been suggested as a risk factor for developing PTCS. The aim of this study was to determine the prevalence and risk factors for developing PTCS among pediatric kidney transplant recipients.
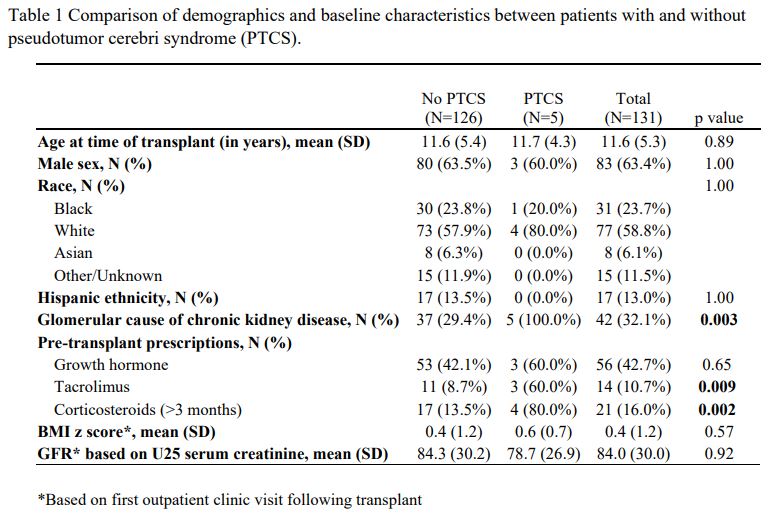
Methods: This cohort study included all pediatric patients (<21 years) who received a kidney transplant at a single tertiary-care institution between January 2011 and June 2022 with at least 6 months of follow-up. Patients were excluded if they had a multi-organ/ prior solid organ transplant, an anatomic cause of PTCS, or PTCS diagnosis pre-transplant. Diagnosis of PTCS was performed by a pediatric neuro-ophthalmologist and papilledema on exam. Demographic and clinical data, including BMI Z-score, pre- and post-transplant medication exposure (steroids, growth hormone, tacrolimus), renal disease etiology, age at transplant, and kidney function (U25 eGFR based on serum creatinine) were assessed for their associations with PTCS by comparing between those with vs. without developing PTCS using two-sample t-test for continuous measures and Fisher’s exact test for categorical measures.
Results: One hundred thirty-one patients met inclusion criteria, of which 5 (3.8%, 95% Confidence interval: 1.3%-8.7%) developed PTCS. Four out of 5 (80%) presented with concerning symptoms (progressive headaches and/or visual disturbances) and 1 was incidentally identified during screening for CMV retinitis. Of those with PTCS, 3 (60%) were male, 5 (100%) had a glomerular etiology for their kidney disease, mean age at transplant was 11.7 years; and they developed PTCS between 9 and 77 months post-transplant (mean = 26 months). Compared to patients without developing PTCS, those with PTCS were more likely to have a glomerular cause of renal disease (100% vs 29%, p=0.003) and pre-transplant exposure to tacrolimus (60% vs 9%, p=0.009) or steroids (80% vs 14%, p=0.002). No difference between groups were found in other demographic or clinical data.
Conclusion: Pediatric patients undergoing renal transplant are at a higher risk of developing PTCS than the general population. Glomerular disease and associated medications were risk factors for developing PTCS, and most of our patients developed PTCS within two years after transplant. These findings should raise awareness about screening for PTCS in transplanted children who present with complaints of progressive headache and/or visual changes.
The Children's Hospital of Philadelphia Distinguished Endowed Chair in the Department of Pediatrics 910220167 (Dr. Amaral). The Children's Hospital of Philadelphia Richard Shafritz Endowed Chair in Pediatric Ophthalmology Research (Dr. Avery). Pediatric Center of Excellence in Nephrology (PCEN) and the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under award number P50DK114786. We’d like to acknowledge Kiara Mouzon MD for her work on the project while a student in the CHOP PCEN program..
References:
[1] pseudotumor cerebri syndrome
[2] idiopathic intracranial hypertension
[3] kidney transplant
[4] glomerular disease
[5] immunosuppression
[6] pediatrics
[7] monitoring post-transplant
[8] ophthalmology
