
Contemporary treatment responses of recurrent focal segmental glomerulosclerosis or steroid resistant nephrotic syndrome in children after kidney transplantation: Phase 2 of a multicenter electronic health record data analysis
Vikas Dharnidharka1, Asha Moudgil2, Priya Verghese3, Leyat Tal4, Rebecca Scobell5, Mahmoud Kallash6, Amy Goodwin Davies5, Nicole Marchesani5, Mitchell Maltenfort5, Megan Kelton7, Margret Bock8, Eliza Blanchette8, Hillarey Stone9, Caroline Gluck10, Frank Hullekes11, Leonardo Riella11, William Smoyer6, Mark Mitsnefes9, Bradley Dixon8, Joseph Flynn7, Michael Somers12, Christopher Forrest5, Susan Furth5, Michelle Denburg5.
1Pediatrics, Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ, United States; 2Children's National Medical Center, Washington DC, United States; 3Ann and Robert Lurie Children's Hospital, Chicago, United States; 4Texas Children's Hospital, Houston, United States; 5Children's Hospital of Philadelphia, Philadelphia, United States; 6Nationwide Children's Hospital, Columbus, United States; 7Seattle Children's Hospital, Seattle, United States; 8Children's Hospital of Colorado, Denver, United States; 9Cincinnati Children's Hospital, Cincinnati, United States; 10Nemours Children's System, Wilmington, United States; 11Massachusetts General Hospital, Boston, United States; 12Children's Hospital, Boston, United States
Background: In a prior phase 1, we reported risk factors for recurrence of focal segmental glomerulosclerosis r(FSGS) or steroid-resistant nephrotic syndrome (SRNS) after kidney transplant but favorable outcomes in a contemporary 7 center cohort. In phase 2, four additional centers have contributed data on treatments and outcomes after rFSGS.
Methods: We applied computational phenotypes to electronic health records aggregated data from 11 large pediatric health systems in the USA, to identify treatments used, typically in non-random fashion, and outcomes. We refined the data collection by chart review. We performed both linear and non-linear Cox regression multivariable analyses with penalized splines to allow for time-varying predictors.
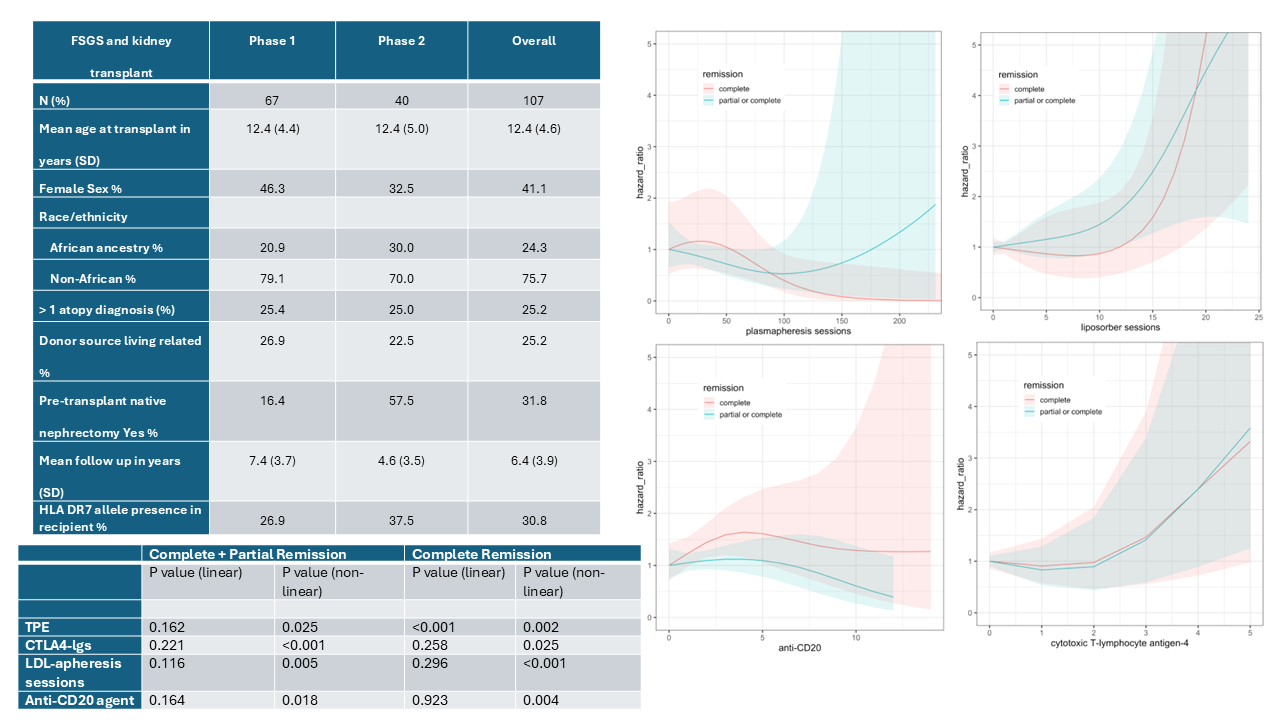
Results: To our original rFSGS cohort of 67, we have now added data on 40 more patients (Figure upper table). Most clinical characteristics were similar between cohorts 1 and 2, except for high rate of native nephrectomy and shorter mean follow up time in cohort 2. Plasmapheresis was used in 101/107 patients, followed by anti-CD20 agents in 84, and Low Density Lipoprotein (LDL)-apheresis in 22. In linear multivariable models, only more plasmapheresis sessions were associated with only complete remission (Figure lower table). But in non-linear models, more doses or sessions of all the above treatments were associated with complete remission alone, or complete + partial remission. Penalized spline curves for complete or complete + partial remission hazard showed greatest yield within 5 doses of antiCD20 agents but increasing yield with more doses/sessions of CTLA4Igs or LDL-apheresis (Figure panels to right). A limitation of the retrospective analysis is that number of doses/sessions may increase until the patient responds.
Conclusions: The results suggest favorable outcomes with increased doses/sessions or additional therapies. Non-linear modelling may help identify the number of doses/sessions at which further increases do not improve outcomes. These retrospective results may inform the design of a randomized study.
This research was funded by a Pilot Grant from The Children’s Hospital of Philadelphia Pediatric Center of Excellence in Nephrology and the NIH/NIDDK under award number P50 DK1147786, PCORnet CRN-2020-007 and PCORI Award 1306-01556.
[1] Focal segmental glomerulosclerosis
[2] Kidney Transplant
[3] Recurrent disease