Devprakash Choudhary, India has been granted the TTS Congress Scientific Awards

Dr. Devprakash Choudhary is India's first surgeon to be awarded an M.Ch in Organ Transplantation. He currently serves as an Assistant Professor in the Department of Renal Transplant Surgery at PGIMER Chandigarh, India’s premier kidney and pancreas transplantation institution, and the national apex center for pancreas transplantation. An alumnus of AIIMS New Delhi (MS) and PGIMER (M.Ch), Dr. Choudhary also served as an IPTA Multi-Organ Transplant Fellow.
His clinical and academic interests are focused on pediatric, multiorgan, and pancreas transplantation. Passionate about advancing the field, Dr. Choudhary’s research emphasizes expanding the donor pool, improving long-term graft survival, and translating scientific innovation into practical, patient-centered transplant care.
Dr. Choudhary has earned more than a dozen prestigious international awards in recognition of his contributions to transplant surgery. He is an invited peer reviewer for high-impact transplant journals and international conferences, and an active member of leading professional societies, including The TTS, ASTS, ESOT, IPTA, and the IPITA.
Beyond the operating room, Dr. Choudhary is a committed academician, long-distance runner, yoga practitioner, and boxing enthusiast.
Pediatric vs. adult living donor kidney transplantation: A comparative analysis from a high-volume tertiary center
Devprakash Choudhary1, Rohan Rao1, Enaganti Ramkishan Rao1, Karalanglin Tiewsoh2, Lesa Dawman2, Jasmine Sethi3, Shivakumar SP1, Deepesh Kenwar1, Sarbpreet Singh 1, Ashish Sharma1.
1Department of Renal Transplant Surgery , PGIMER, Chandigarh, India; 2Department of Pediatric Nephrology, PGIMER, Chandigarh, India; 3Department of Nephrology , PGIMER, Chandigarh, India
Introduction: Although Pediatric kidney transplantation poses unique anatomical, immunological, and psychological challenges, it offers excellent long-term survival and quality of life benefits. However, comparative data from resource-limited countries remain sparse. This study compares perioperative characteristics and transplant outcomes between pediatric and adult recipients undergoing living donor kidney transplantation (LDKT) at a high-volume transplant center.
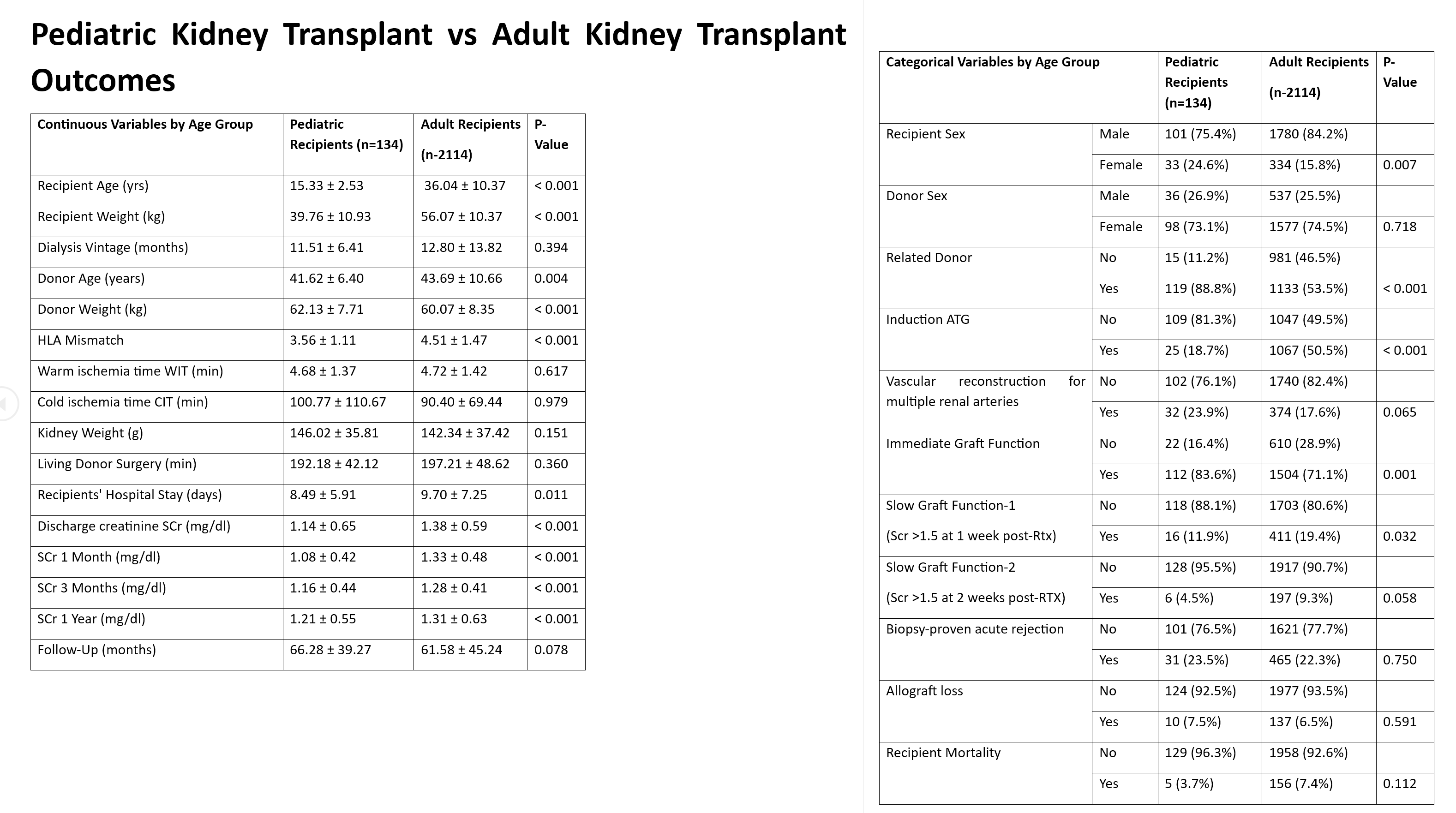
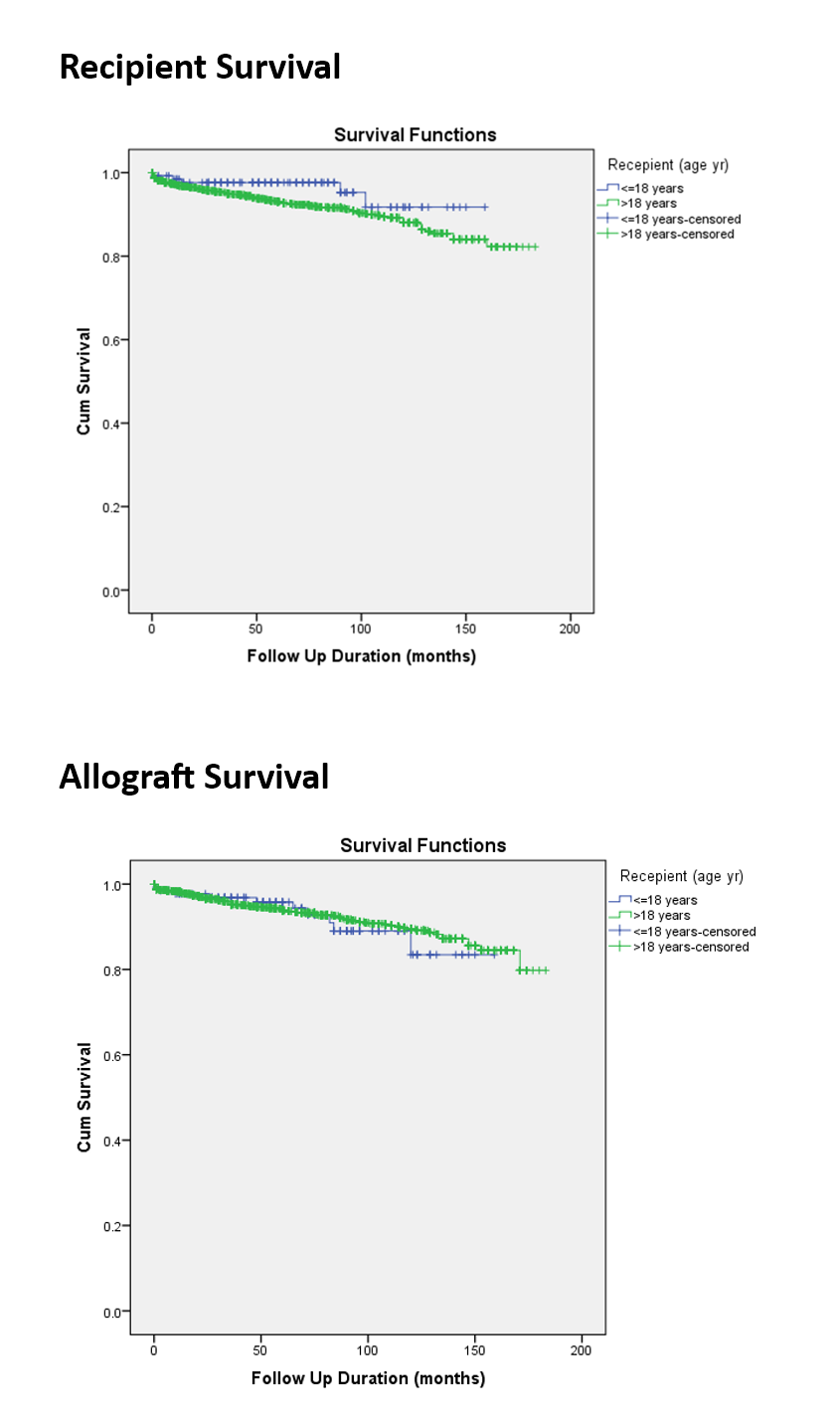
Methods: This retrospective comparative study involved 134 pediatric recipients (≤18 years) and 2,114 adult living donor kidney transplant recipients (KTRs) who underwent transplantation between September 2008 and December 2022. Clinical, surgical, and follow-up data were obtained from prospectively maintained electronic departmental databases. Recipients were compared across demographic, intraoperative, and postoperative parameters. Primary outcomes included graft function, allograft rejection, graft loss, and patient survival, with a mean follow-up of 5 years. Missing data were handled using pairwise deletion during analysis, and no imputation was performed.
Results: Pediatric recipients exhibited significantly better early graft function, with improved eGFR at discharge (p<0.001), and at 1 month (p<0.001), 3 months (p<0.001), and 1 year (p<0.001). Immediate graft function was more frequent in pediatric recipients (p = 0.001), with shorter hospital stays (p = 0.011). Pediatric recipients also had significantly lower HLA mismatches (p<0.001) and a higher proportion of related donors (p<0.001). Despite significantly lower ATG induction (18.7%) in pediatric recipients, rates of biopsy-proven acute rejection (23.5% vs. 22.3%), graft loss (7.5% vs. 6.5%), and mortality (3.7% vs. 7.4%) were statistically comparable to adult LDKT.
Conclusion: Consistent with the international literature, pediatric kidney transplants (KTRs) at our center achieved optimal graft function and comparable survival outcomes to those of adult KTRs despite low ATG induction rates, which reinforces the viability of pediatric transplantation in low-resource settings. Favorable donor-recipient profiles, surgical experience, and multidisciplinary care likely contributed to these outcomes. Emphasis on early referral and adolescent-focused support may further enhance long-term success.
We sincerely acknowledge the invaluable support and dedication of the transplant coordinator team, whose tireless efforts in recipient coordination and logistical planning were instrumental to the success of this transplant program..
[1] Allograft Survival
[2] Graft Rejection
[3] ATG Induction
[4] Pediatric Kidney Transplant