
Professor Stephen Marks, MD MSc MRCP DCH FRCPCH is Professor of Paediatric Nephrology and Transplantation at University College London Great Ormond Street Institute of Child Health and President of the British Association for Paediatric Nephrology. He is clinical lead for renal transplantation and Director of the National Institute for Health Research Great Ormond Street Hospital Clinical Research Facility at Great Ormond Street Hospital for Children NHS Foundation Trust. He has local, national and international roles including Chair of the Education Committee of the International Pediatric Transplant Association (IPTA) having also been an IPTA Councillor. His research continues to date in the fields of renal transplantation (including innovative drug trials concerning new anti-rejection therapies and assessment of children post-renal transplantation), systemic lupus erythematosus and vasculitis. He is on the editorial board for “Pediatric Nephrology” and “British Journal of Renal Medicine” and is associate editor for “Transplantation” and “Pediatric Transplantation”, which are the journals of The Transplantation Society (TTS) and the International Pediatric Transplant Association (IPTA), respectively.
Longitudinal European Paediatric Access to Kidney Transplantation (EuPAKT) study with the CERTAIN registry
Jisoo Kim1,2, Kai Krupka3, Burkhard Tonshoff3, Stephen Marks1,2.
1Department of Paediatric Nephrology, Great Ormond Street Hospital for Children NHS Foundation Trust, London, United Kingdom; 2NIHR Great Ormond Street Hospital Biomedical Research Centre, University College London Great Ormond Street Institute of Child Health, London, United Kingdom; 3Deparment of Paediatric Nephrology, University Children's Hospital, Heidelberg, Germany
Introduction: Kidney transplantation is the gold standard kidney replacement therapy in optimising health and improving quality of life in children with Stage 5 Chronic Kidney Disease (CKD-5). However, multiple factors, including psychosocial and therapy adherence, have been cited to delay transplantation. Moreover, we do not understand how transplantation delays influence the child’s quality of life (QoL).
Aim: We explored the factors delaying paediatric kidney transplantation across Europe, in particular psychosocial factors including therapy adherence. We aimed to (1) understand the influence of psychosocial factors on transplantation time relative to other factors cited to delay transplantation and (2) examine changes in QoL and therapy adherence over time.
Methods: A multicentre, longitudinal registry study of 11 European paediatric nephrology centres was designed to prospectively collect pre-transplantation data on all patients receiving paediatric care with CKD-5 over 12 months, followed by one year post-baseline data. We collected data on patient demographics, clinician-reported factors delaying transplantation, changes in kidney replacement therapy including transplantation during the study period, patient- and proxy-reported QoL and clinician-, patient- and proxy-reported therapy adherence all on a 1 to 5 Likert scale.
Results: Among 167 patient entries, 156 (93%) had adequate follow-up data for preliminary analysis and among patients with follow-up data, 53 (34%) had received a kidney transplant during the study period. There were 203 entries describing factors contributing to kidney transplantation delay. The most cited factors were donor availability (41.9%), disease-related (23.6%), size of the child (11.8%) and psychosocial (10.8%). Children having “psychosocial factors” delaying their transplant at baseline, were less likely to be among the children who received a kidney transplant (p = 0.02). At pre-transplant baseline, there was no difference in clinician-, patient- or carer-reported therapy adherence between those who later received a transplant and those who did not. Transplanted children were more likely to report a better QoL score at pre-transplant baseline than those who did not (p = 0.03). We examined therapy adherence and QoL over time in children who did not receive a transplant. Although there was no significant difference in therapy adherence (clinician-reported p = 0.7, patient-reported p = 0.3, carer-reported p=0.8), QoL scores declined after one year of waiting for a transplant (patient-reported p = 0.006, carer-reported p < 0.001).
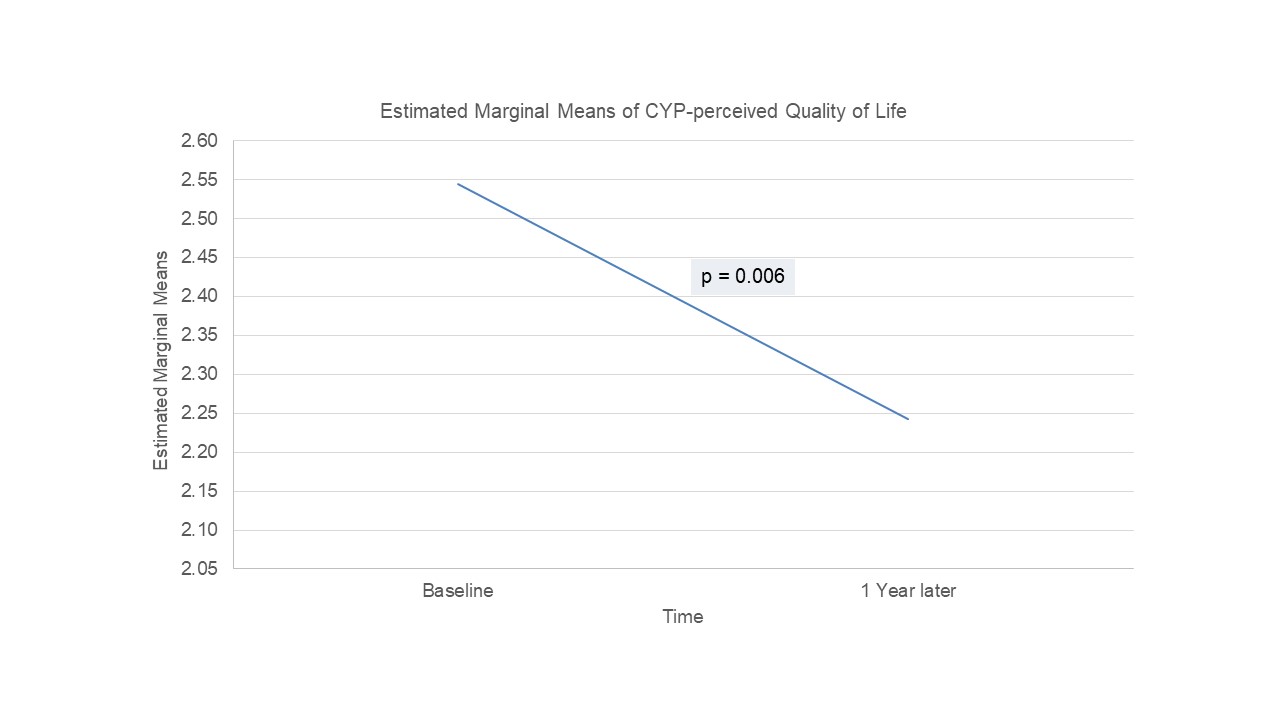
Conclusion: Children with psychosocial factors delaying transplantation are more likely to experience greater delays in transplantation than those without. There is no difference in therapy adherence between children who receive a transplant and those who experience delays. Children waiting more than one year for kidney transplantation are likely to experience significant decline in their QoL.
The authors are grateful for all of the CERTAIN Registry sites that took part including all of the patients and their families.
[1] transplantation delays
[2] psychosocial factors
[3] therapy adherence
[4] longitudinal study
[5] European study