Alejandro Zarauza Santoveña, Spain
Attending Physician
Pediatric Nephrology
Hospital Universitario La Paz
Successful treatment of relapsing focal and segmental glomerulosclerosis using immunoadsorption and B-cell targeted therapy
Alejandro Zarauza Santoveña1, Carlota Fernández Camblor1, Leticia Ramos Macías2, Diego Morante Martínez1, Laura García Espinosa1, Juan Bravo Feito1, Marta Melgosa Hijosa1.
1Pediatric Nephrology, Hospital Universitario La Paz, Madrid, Spain; 2Pediatric Nephrology, Complejo Hospitalario Universitario Insular Materno-Infantil. , Las Palmas de Gran Canaria, Spain
Introduction: Recurrence of primary focal and segmental glomerulosclerosis (FSGS) is common after kidney transplant (KTx), and significantly impacts graft prognosis. When proteinuria control is not achieved, the risk of graft loss is high. First line of therapy includes apheresis techniques and B-cell-targeted therapies, including recent case reports employing a global B-cell strategy with anti-CD20 and anti-CD38 antibodies.
Methods: case report of an early FSGS recurrence succesfully treated with immunoadsortion (IA) and anti-B-cell therapy with obinutuzumab (anti-CD20) and daratumumab (anti-CD38).
Results: 11 y girl. Debut of steroid-resistant nephrotic síndrome at 4 y. Partial response to cyclosporine during 18m, after which she has a relapse with no response to any immunosupression (IS) received: steroids, cyclosporine, tacrolimus (TAC), micophenolate (MMF) and rituximab. Kidney biopsy showed FSGS with C1q deposit and genetic test was negative. Progressive decline of kidney function, starting hemodialysis at 10 y.
In july 2024 she receives a cadaveric KTx (5/6 HLA missmatches). Standard IS with basiliximab, setroids, TAC and MMF. No surgical complications and good kidney function, serum creatinine (SCr) at discharge 0,6 mg/dL. 2 weeks after KTx nephrotic range proteinuria is detected, with mildly decreased serum albumin, no edema. Therapeutic plasma exchanges (TPE) every 48h are initiated. Proteinuria rapidly improves, but rises when TPE is spaced out. After 10 TPE we decided to change to IA (TheraSorb Ig omni 5) 3 times/week. We added a single dose of obinutuzumab (20 mg/kg) at +10 w because of anafilaxy during a rituximab infusión at +6w, and completed treatment with 3 doses of daratumumab (16 mg/Kg/dose in a split 2-day infusión, figure 1). Antiproteinuric therapy with losartan is started and TAC is adjusted to trough levels 7-9 ng/mL. Infectious prophylaxis with co-trimoxazol and valganciclvoir was added. IA was stopped after 20 sessions. Patient is stable with mild proteinuria and normal SCr.
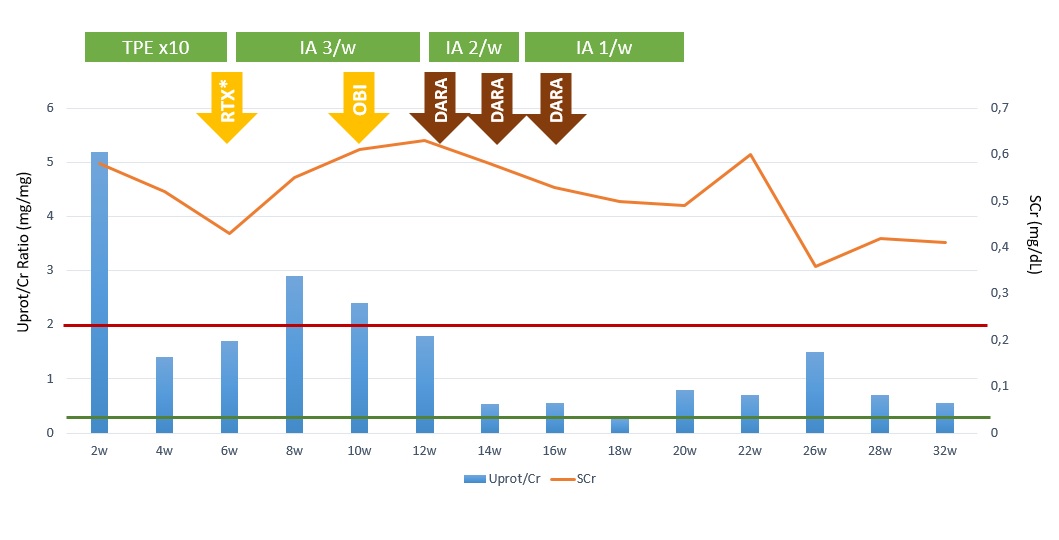
As adverse effects, she developed transient moderate neutropenia, persistent hypogammaglobulinemia and asymptomatic CMV primary infection at +30 w (after valganciclovir discontinuation due to neutropenia). At +32 w, she maintains CD19-20 cell depletion.
Conclusion: Combined treatment with IA and anti-B-cell antibodies seems to be a good combination for the treatment of FSGS recurrence post KTx. In our patient we achieved good control of proteinuria. Special care must be taken with regard to adverse effects and high risk of infection.
References:
[1] FSGS recurrence
[2] Kidney transplant
[3] Immunosuppression
