Vindya N Gunasekara Sr., Sri Lanka
Consultant Paediatric Nephrologist
Paediatric Nephrology
Lady Ridgeway Hospital For Children
The first cohort of paediatric kidney transplant recipients with hostile bladder in Sri Lanka
Vindya N Gunasekara1, Thilini Pathirage1, Mandika Wijerathne2, Rizni Cassim2, Harshani P Warnakulasooriya3, Maithili Luxman1, Ananda Lamahewage4, Neville Perera5.
1Paediatric Nephrology, Lady Ridgeway Hospital For Children, Colombo 08, Sri Lanka; 2Department of Surgery , University of Colombo, Colombo, Sri Lanka; 3Medical Administration, National Hospital Sri Lanka, Colombo 08, Sri Lanka; 4Department of Surgery , Lady Ridgeway Hospital For Children, Colombo 08, Sri Lanka; 5Department of Urology, National Hospital Sri Lanka, Colombo 08, Sri Lanka
Introduction: In 2009, Sri Lanka’s first paediatric urodynamic and bladder training unit was established at the Department of Nephrology of Lady Ridgeway Hospital for Children, LRHC, improving the preservation of renal function in children with bladder disorders. In the absence of specialized paediatric urology support, children with end-stage renal disease and hostile bladders were prepared for kidney transplantation (KT) in collaboration with adult urologists and paediatric surgeons, amidst many challenges. This study compared outcomes of paediatric kidney transplant recipients (PKTRs) with hostile bladders versus those with normal bladder functions in a low-resource setting.
Method: Data of all paediatric PKTRs in the nephrology unit, LRHC, since its initiation (from 2016-2024), were retrospectively analyzed. A hostile bladder was defined as a high-pressure, retentive bladder needing clean intermittent catheterization (CIC).
Post-KT outcome parameters included urinary tract infections (UTI), survival rates, rejection episodes, and estimated glomerular filtration rates (eGFR). Statistical tests included One-way ANOVA, and Chi-square tests. Additionally, Poisson regression and Kaplan-Meier analysis were used to compare infection rate ratios (IRR) and survival rates, respectively. A P value of <0.05 was considered significant.
Results: Eleven children had hostile bladders (Group 1) (median age 13.5 (IQR 4-16); median follow-up 3.1 (IQR 0.01-6.3) years. Primary bladder pathologies included posterior urethral valve (n=6), neurogenic bladder (n=3), and non-neurogenic neurogenic bladder (n=2). Two children had VACTERL anomalies. All had trabeculated high-pressure or retentive bladders pre-transplant, 9/11 needed bladder augmentation, and all required nephroureterectomy. After 6 months, post-KT, 8/10 patients reused the CIC catheters.
Group 1 was compared to 31 children with normal voiding (Group 2). (Figure 1) During the first three months post-transplant, UTIs occurred in 5/10 in Group 1 versus 1/30 in Group 2. The UTI rate per patient-year was significantly higher in Group 1 (0.5 versus 0.06) (IRR 9.2 (95% CI: 3.6 – 23.3, p < 0.001). Four patients in Group 1 required further bladder surgeries after KT, compared to none in Group 2. At 3 years, patient survival in Group 1 was 100% and graft survival was 90.9% (95% CI 73.8 – 108.0%). Survival rates, 3-year eGFR, and rejection rates were similar in both groups.
" href="https://app.ipta2025.org/papers/body/362#">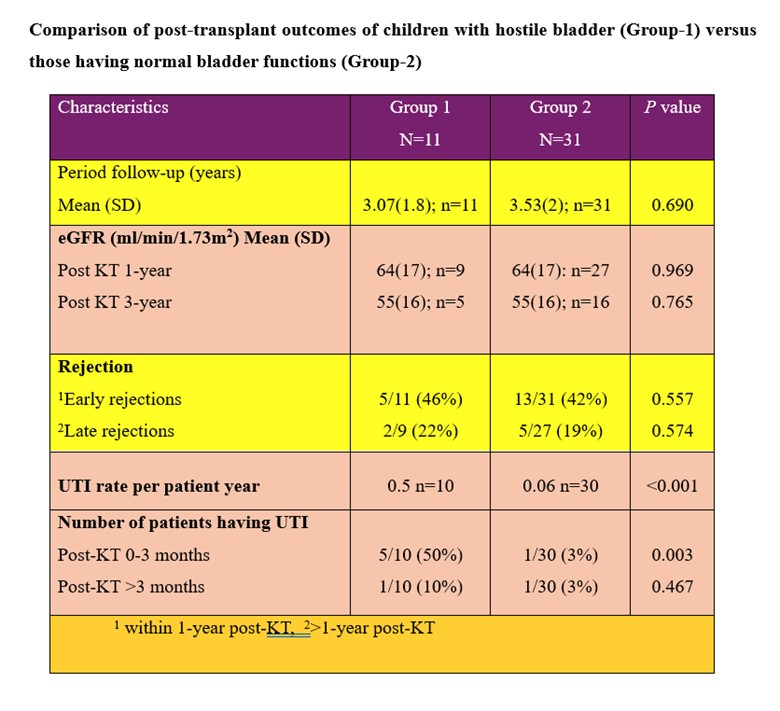
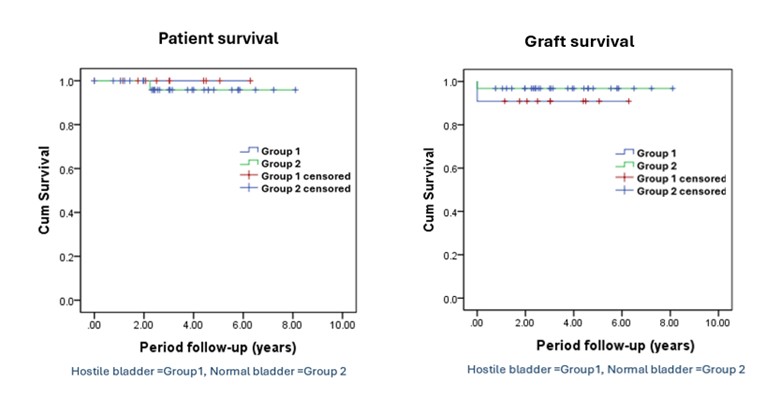
Conclusion: Children with hostile bladders had significantly higher UTI rates and had more post-surgical complications. However, UTI risk decreased after 3 months despite reusing the CIC catheters. Furthermore, there were no notable differences in medium-term patient survival, graft survival, or eGFR compared to children with normal bladder functions. These results suggest that satisfactory outcomes are achievable for paediatric kidney transplant recipients with hostile bladders even in low-resource settings.
References:
[1] paediatric kidney transplant
[2] hostile bladder
[3] outcomes
[4] low resource countries
Lectures by Vindya N Gunasekara Sr.
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Fri-19 11:05 - 12:05 |
Breaking down barriers to transplant in low resource settings | Panel discussion on the challenges of access to transplant and innovative solutions: South Asian perspective | MOA 3 |
|
Thu-18 17:00 - 18:00 |
Kidney Posters - from P1.1 to P1.32 | Outcomes of paediatric kidney transplant: A single centre experience from Sri Lanka | MOA 10 (Exhibit Area) |
|
Thu-18 17:00 - 18:00 |
Kidney Posters - from P1.1 to P1.32 | The first cohort of paediatric kidney transplant recipients with hostile bladder in Sri Lanka | MOA 10 (Exhibit Area) |
