Vindya N Gunasekara Sr., Sri Lanka
Consultant Paediatric Nephrologist
Paediatric Nephrology
Lady Ridgeway Hospital For Children
Outcomes of paediatric kidney transplant: A single centre experience from Sri Lanka
Vindya N Gunasekara sr1, Thilini Pathirage jr1, Maithili Luxman jr1, Mandika Wijerathne sr2, Rizni Cassim sr2, Anuja Abayadeera sr3, Harshani P Warnakulasooriya4.
1Paediatric Nephrology, Lady Ridgeway Hospital For Children, Colombo 08, Sri Lanka; 2Department of Surgery , University of Colombo, Colombo, Sri Lanka; 3Department of Anaesthesiology, University of Colombo, Colombo 08, Sri Lanka; 4Community Medicine, Ministry of Health, Colombo, Sri Lanka
Introduction: Despite excellent survival statistics reported in developed world paediatric post-transplant mortality rates are still high in resource-poor settings. This study aims to analyse the outcomes of the renal transplant programme initiated in 2016, at Lady Ridgeway Hospital for Children (LRHC) in Sri Lanka.
Method: Data of 41 children (68% boys) who received renal transplantation and were managed by the paediatric nephrology team in LRHC from 2016 to 2024 were extracted from the database of the unit. All donor kidneys were harvested in an adult centre, and recipient surgeries were performed at LRHC (36/41) or in an adult centre (5/41). All patients received anti-interleukin-2 receptor inhibitors at induction, and mycophenolic acid, tacrolimus, and prednisolone as maintenance treatment.
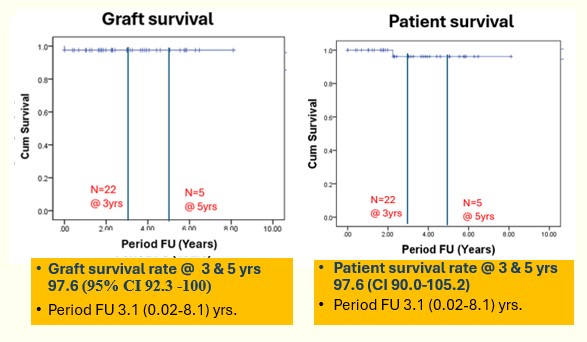
Outcome parameters included graft and patient survival rates, rejection episodes, and 3-year post-transplant estimated glomerular filtration rates (3YeGFR). Survival rates were calculated using Kaplan-Meier survival analysis. Factors that could have affected the 3YeGFR values were assessed in a linear regression model. p-value <0.05 was considered statistically significant.
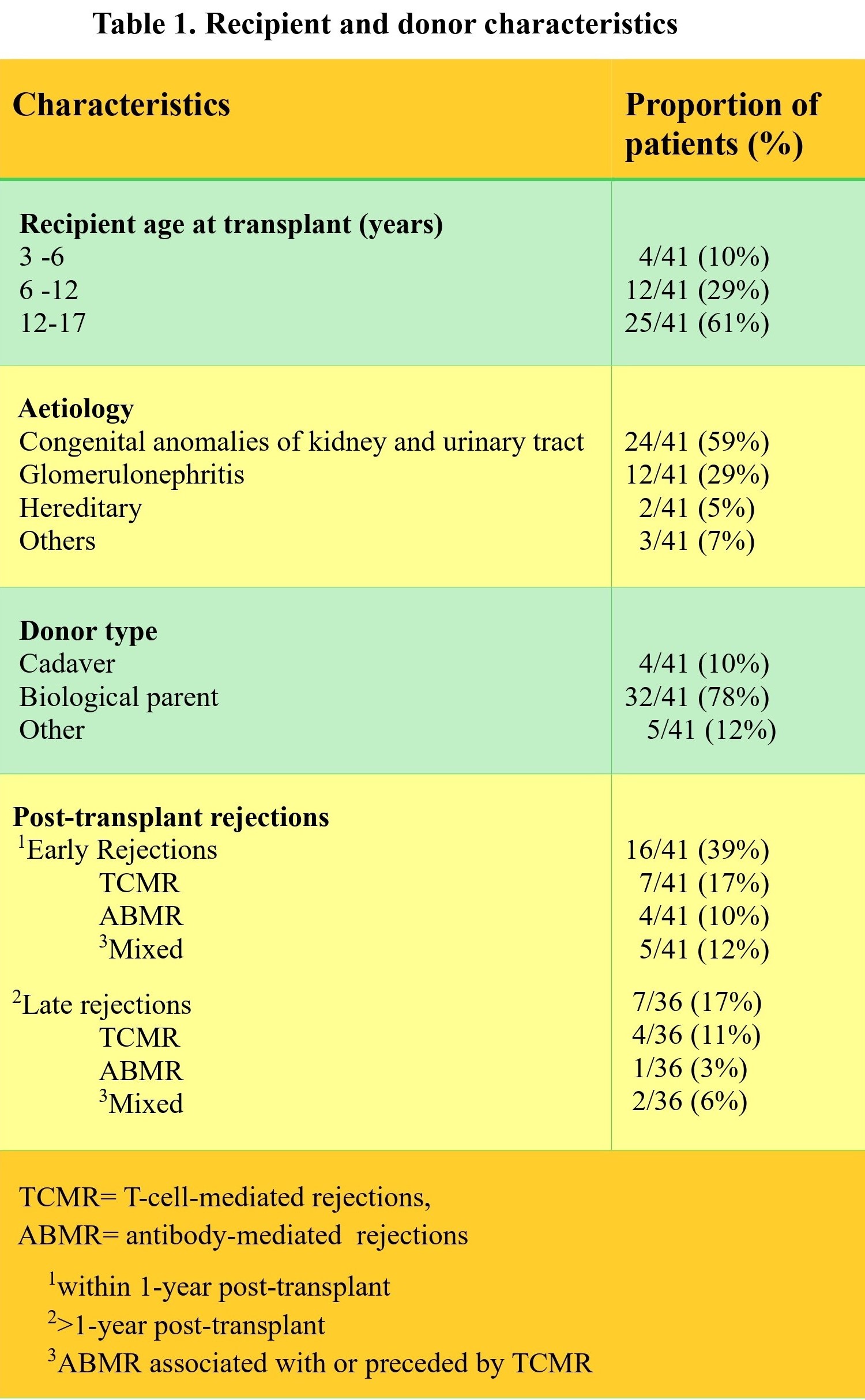
Results: Median (range) age was 13.4 (3.4 -17.6) years, weight was 24.3 (9.8 -55.7) kg, and follow-up was 3.1 (0.02-8.1) years. Only 2/41 received pre-emptive transplants, and 6/41 had delayed graft function. (Table 1.)
One cadaver kidney recipient died after 2.2 years due to sepsis, and one graft was lost due to hyperacute rejection. Graft survival rate was 97.6% (95% CI 92.3 -100), and patient survival rate was also 97.6% (95% CI 90.0-100) at 3 and 5 years. Urinary tract infection was the most common infection (6/41). One child each had BKV nephropathy and CMV disease. Mean (SD) values of post-transplant eGFR at 1 month, 3 years, and 5 years were 80(25), 54(17), and 55(17) ml/min/1.73m2, respectively. Majority with late rejections had previous acute rejection episodes (6/7), and nonadherence to medication (4/7).
Twenty-one patients had completed 3-year follow-up. Mean (SD) 3YeGFR (ml/min/1.73m2) was significantly lower in those with late rejections Vs. without rejections (60(12): 30(14)), and when the donor age was >45 Vs. <45 years (60(15): 40(13)). In multiple linear regression, late rejections (β=25: 95% CI:13-38), and donor age (β=15; 95% CI:5-26) significantly predicted the 3YeGFR, F (2,18) =18.133, p=<0.005, R2=.668
Conclusion: Short and medium-term patient and graft survival rates of the programme are commendable. Rejection episodes were high, and late rejections and donor age were significant predictors of 3YeGFR. These findings highlight the impact of late rejections and donor age on long-term graft function.
Paediatric Nephrology Team LRHC. Dr A Lamahewage. Dr M Samarasinghe. Dr N Perera.
References:
[1] kidney transplant
[2] Sri Lanka
[3] survival rates
[4] paediatric
Lectures by Vindya N Gunasekara Sr.
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Fri-19 11:05 - 12:05 |
Breaking down barriers to transplant in low resource settings | Panel discussion on the challenges of access to transplant and innovative solutions: South Asian perspective | MOA 3 |
|
Thu-18 17:00 - 18:00 |
Kidney Posters - from P1.1 to P1.32 | Outcomes of paediatric kidney transplant: A single centre experience from Sri Lanka | MOA 10 (Exhibit Area) |
|
Thu-18 17:00 - 18:00 |
Kidney Posters - from P1.1 to P1.32 | The first cohort of paediatric kidney transplant recipients with hostile bladder in Sri Lanka | MOA 10 (Exhibit Area) |
