Global perspectives on nonadherence and re-transplantation in pediatric solid organ transplant recipients: An IPTA Ethics committee analysis
Katheryn Gambetta MD1, Megha D Tandel MPH2, Mihaela A Damian MD3, Mignon McCulloch MBBCH4, Debra Lefkowitz PsyD5, Tom D Blydt-Hansen MDCM6.
1Pediatric Heart Failure & Heart Transplant, Ann & Robert H Lurie Children's Hospital, Chicago, IL, United States; 2Quantitative Sciences Unit, Stanford Hospital, Palo Alto, CA, United States; 3Pediatric Critical Care, Emory University School of Medicine, Atlanta, GA, United States; 4Pediatric Nephrology & Solid Organ Transplantation, Red Cross Children's Hospital, Cape Town, South Africa; 5Department of Adolescent & Child Psychiatry, Children's Hospital of Philadelphia, Philadelphia, PA, United States; 6Multi-Organ Transplant Program, BC Children's Hospital, Vancouver , BC, Canada
Background: Nonadherence in pediatric transplant patients is a significant challenge that increases risk of rejection, graft failure, and re-transplantation for which nonadherence may be considered a contraindication. We investigated the global impact of pediatric nonadherence with goal of understanding ethical issues regarding re-transplantation worldwide.
Methods: In 2023, the IPTA Ethics committee conducted anonymous online survey (REDCap) of IPTA members, consisting of 42 questions addressing participant demographics, definitions of adherence to medications and clinic appointments, and practice patterns. Responses were reported using standard descriptive statistics. Univariate analyses were performed to assess significance of primary outcomes by country.
Results: Seventy of 936 IPTA members (7.5%) from 19 countries completed the entire survey; majority were physicians (74.3%). Participants were from these country groups: Americas defined as countries from North, Central and South America (n=47, 67.1%), followed by European (n=12, 17.1%), Asian/Pacific (n=7, 10.0%) and Middle East/African countries (n=4, 5.7%). Majority of participants were from countries of high gross national income (GNI) (84.3%). Median global inequality index for participants was 39.8% (IQR 32.9-39.8)(Table 1).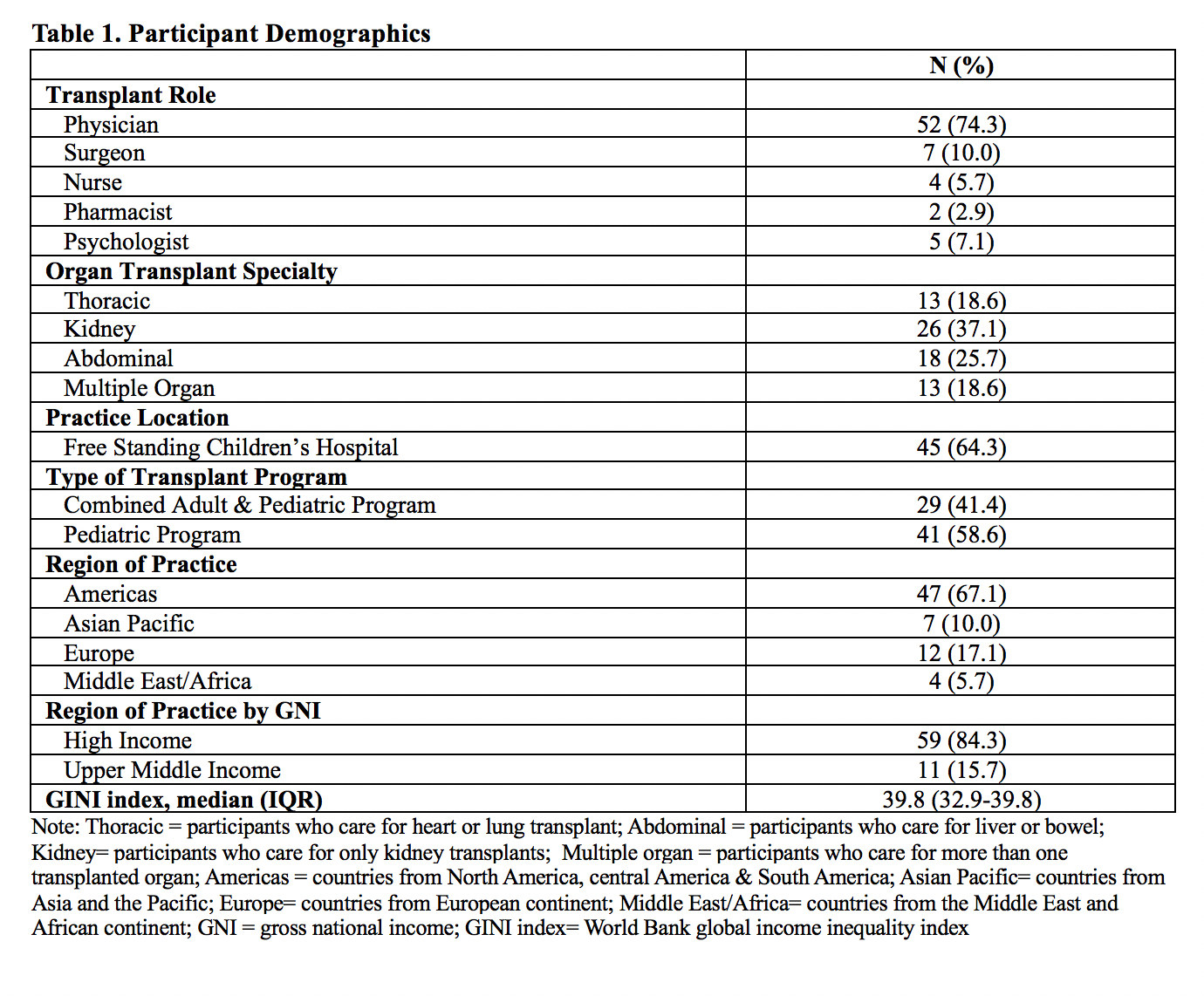
Overall reported nonadherence was common with medications (15%, IQR 5-30%) and clinic appointments (10%, IQR 5-15%). Medication nonadherence definition differed slightly with 1 missed dose of immunosuppressants a week considered detrimental in European countries (50%), while 2 missed doses a week in Americas (43%), and ≥ 3 missed doses a week in Asian/Pacific (71%) and Middle East/African countries (67%) were considered detrimental (p=0.11). Although not significant, median age (years) at which patients can be independently responsible for medications varied from the Americas considering 17 an appropriate age (p=0.07), while other country groups considered age of 16 (IQR 15-18)(p=0.11). Median of 3 missed clinic appointments a year (IQR 2-3) was considered significant among all countries. 13% of participants from Americas have policy addressing nonadherence while other countries do not. When medication nonadherence contributed to graft failure, 50% participants from Europe would offer re-transplant, followed by 30% from Americas, 29% from Asian/Pacific, and 0% from Middle East/African countries. No participants consulted ethics in decisions regarding eligibility. Age of child was factor in determining eligibility in participants from Americas and Europe, but not other countries (p=0.03). Interventions to support eligibility for re-transplant include psychology and social work involvement and increased clinical monitoring (Figure 1).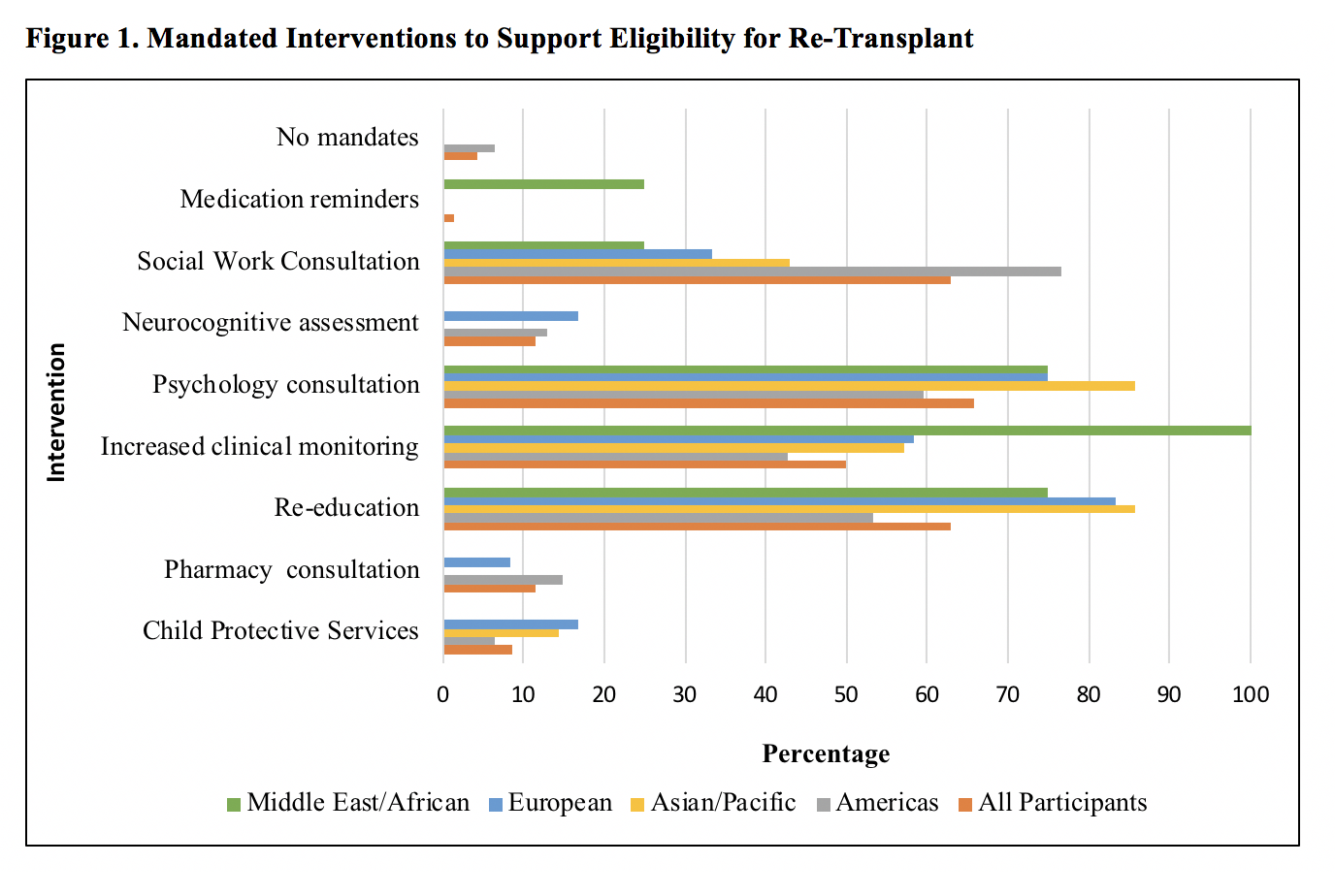
Conclusion: Nonadherence continues to be problematic globally. Defining medication non-adherence, expectations for independent self-care, and interventions to promote adherence are similar worldwide.
References:
[1] ethics
[2] nonadherence
[3] re-transplantation
