Organ specific considerations regarding re-transplantation after nonadherence: An IPTA ethics committee analysis
Katheryn E Gambetta1, Megha Tandel2, Mihaela Damian3, Mignon McCulloch4, Debra Lefkowitz5, Anna Gold6, Clare J Lindner7, Sanjay Rao8, Tom Blydt-Hansen9.
1Heart Failure & Heart Transplant, Ann & Robert H Lure Children's Hospital, Chicago, IL, United States; 2Quantitative Sciences Unit, Stanford Hospital, Palo Alto, CA, United States; 3Pediatric Critical Care, Emory University School of Medicine, Atlanta, GA, United States; 4Pediatric Nephrology & Solid Organ Transplantation, Red Cross Children's Hospital, Cape Town, South Africa; 5Department of Child & Adolescent Psychiatry, Children's Hospital of Philadelphia, Philadelphia, PA, United States; 6Department of Psychology, The Hospital for Sick Children, Toronto, ON, Canada; 7Pediatric Nephrology, C.S. Mott Children's Hospital, Ann Arbor, MI, United States; 8Department of Pediatric Surgery, Mazumdar Shaw Multispecialty Hospital, Bangalore, India; 9Multi-Organ Transplant Program, BC Children’s Hospital, Vancouver, BC, Canada
Introduction: Nonadherence poses consequences for all solid organ pediatric transplant recipients by leading to end stage graft dysfunction and possible need for re-transplantation. Ethical concerns arise when determining candidacy for re-transplantation but may differ based on transplanted organ. Minimal data exists on defining nonadherence and clinical decision-making regarding re-transplantation among organ specialties. We aimed to compare provider perspectives and practices on nonadherence by organ specialty.
Methods: The IPTA Ethics committee conducted an anonymous online survey (REDCap) of IPTA members in 2023 addressing demographics, definitions of adherence to medications and clinic appointments, and practice patterns. Responses were reported using standard descriptive statistics. Univariate analyses were performed to assess significance of primary outcomes by organ transplant specialty.
Results: Seventy of 936 IPTA members (7.5%) from 19 countries completed entire survey; majority were physicians (74.3%). Majority of participants were involved in care of one organ transplant specialty as follows: kidney (37.1%), abdominal (liver or bowel) (25.7%), and thoracic (heart or lung) (18.6%). 18.6% of participants cared for more than one transplanted organ. Median duration of practice for participants was 17 years (IQR 8-25). Additional demographics are shown in Table 1.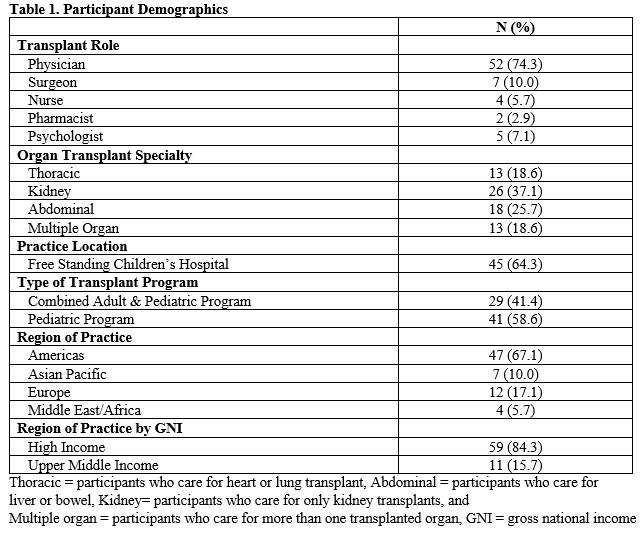
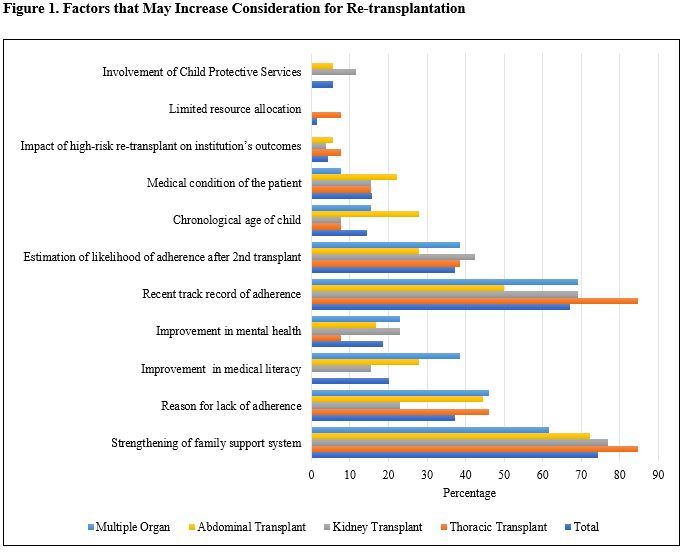
Reported nonadherence occurred frequently in all organ transplant specialty groups with medications (15%, IQR 5-30%) and clinic appointments (10%, IQR 5-15%). Only 37.9% of participants considered two missed doses of immunosuppressants a week a clinically important episode of nonadherence; this was not statistically different among organ transplant specialty groups (p=0.19). Nonadherence with clinic appointments was considered clinically important at median of 2 missed clinics a year (IQR 2-3). Median age of 16 (IQR 15-18) was considered age that patients can be responsible for medications and median age of 18 (IQR 16-18) was considered age that patients are capable to attend visits independently across all transplant groups. Most centers (84%) do not have policy regarding nonadherence. When nonadherence with medications contributed to graft failure, 22 (31.9%) would offer re-transplant but differed by organ transplant specialty (thoracic 0%, kidney 32%, abdominal 44.2%, multiple organs 46.2%; p=0.01). Interventions addressing nonadherence varied focusing on education (85.7%), increased monitoring (81.4%) and counseling (42.9%). Recently improved adherence and strengthening of family support were most frequent considerations for re-transplantation eligibility (Figure 1).
Conclusion: Nonadherence continues to be problematic regardless of transplanted organ. Variability exists in defining non-adherence, expectations for independent self-care and eligibility for re-transplantation. Further work is needed to develop preventive strategies.
References:
[1] nonadherence
[2] graft failure
[3] re-transplantation
[4] ethics
