Cedars-Sinai Medical Center
Risk factors for loss of varicella immunity after pediatric kidney transplantation
Helen Pizzo1, Priya R Soni2, Santhosh Nadipuram2, James Mirocha3, Jonathan Garrison1, Sherlyn Hilario1, Irene K Kim4, Tsuyoshi Todo4, Dechu Puliyanda1.
1Pediatric Nephrology, Cedars-Sinai Guerin Children's, Los Angeles, CA, United States; 2Pediatric Infectious Disease, Cedars-Sinai Guerin Children's, Los Angeles, CA, United States; 3Biostatistics Core, Research Institute , Cedars-Sinai Medical Center, Los Angeles , CA, United States; 4Surgery, Cedars-Sinai Medical Center, Los Angeles, CA, United States
Background: Vaccination against varicella zoster (VZV) before kidney transplant (Tx) can help prevent severe disseminated VZV disease in immunosuppressed patients (Pts) post-Tx. Despite confirmation of serologic response to vaccinations pre-Tx, studies have shown loss of humoral immunity post-Tx. Here we assessed the risk factors for losing VZV immunity after pediatric kidney Tx.
Methods: A retrospective analysis of 45 Pts with positive pre-Tx VZV IgG (> 1.09 index) was performed. Pts received induction with either a lymphocyte depleting (LDA: ATG or alemtuzumab) or a non-lymphocyte depleting agent (NLDA: basiliximab or daclizumab) and maintained on mycophenolate mofetil, tacrolimus, with or without corticosteroids. Loss of VZV immunity (VZV IgG < 1.09 index) post-Tx was evaluated based on 1) the induction agent used 2) the number of VZV vaccines (Vx) received prior to Tx, and 3) the interval between last dose of VZV Vx and Tx.
Results: Median age at Tx was 16.7 yrs (IQR 12.7-18.5); 29 (64.4%) were male; 40 (88.9%) received a deceased donor Tx; and 38 (84.4%) received LDA. Additionally, 34 (75.6%) received two VZV Vx prior to Tx; 10 (22.2%) received their last VZV Vx ≤1 yr prior to Tx. After Tx, 11 (24.4%) Pts lost VZV immunity at a median time of VZV IgG testing at 12.6 mos (IQR 8.8-14.9) post-Tx. Those who lost immunity were younger at the time of transplant, 12.4 yrs (IQR 3.9-17.4) vs. 17.3 yrs (IQR 13.4-19.0) (P=0.004), and more likely to be on steroid-based immunosuppression, 9 (81.8%) vs. 11 (32.4%) (P=0.006). There was no difference in the induction agent used between the two groups (P >0.99). There was an increased risk for losing VZV seropositivity after transplant among those who required 3 or more doses of VZV vaccine to seroconvert prior to Tx (HR 3.81, 95%CI 1.09-13.30, P=0.04). Those who received their VZV Vx <1 yr prior to Tx were more likely to lose post-Tx immunity (Figure 1, P=0.0003). Despite losing immunity, none of the patients developed disseminated VZV.
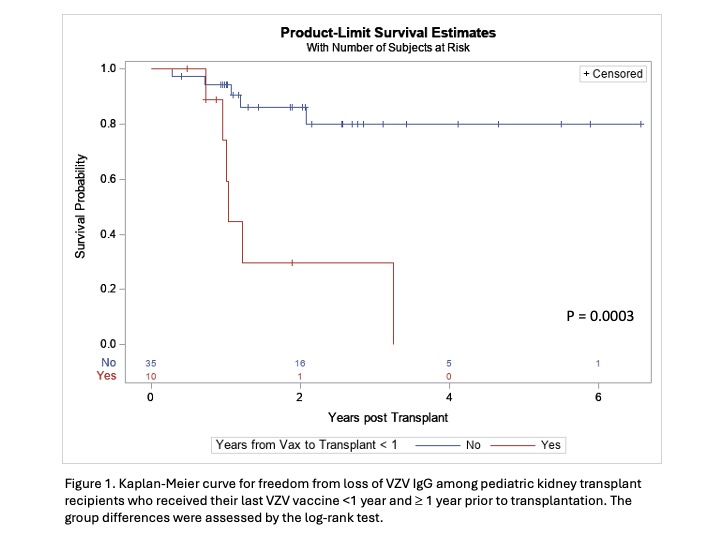
Conclusion: Pediatric kidney Tx Pts are at risk for losing VZV immunity after Tx, with higher incidences among those who were younger at the time of Tx, on steroid-based immunosuppression, required three or more doses of VZV Vx to seroconvert, or received VZV Vx <1 yr before Tx. Post-Tx VZV serologies should be monitored to identify Pts at high risk for disseminated VZV.
References:
[1] Outcomes
[2] Infection
[3] Vaccination
Lectures by Helen Pizzo
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Sun-21 09:15 - 10:45 |
Monitoring after pediatric kidney transplant | Risk factors for loss of varicella immunity after pediatric kidney transplantation | MOA 6 |
|
Sat-20 10:00 - 11:00 |
Optimizing outcomes after pediatric kidney transplantation | Alemtuzumab induction via intravenous vs. subcutaneous administration in pediatric kidney transplantation | MOA 6 |
|
Thu-18 17:00 - 18:00 |
Kidney Posters - from P1.1 to P1.32 | Low incidence of rejection and de novo donor-specific antibody formation following covid-19 vaccination or infection among pediatric kidney transplant recipients | MOA 10 (Exhibit Area) |
