Practice patterns of normothermic machine perfusion use in pediatric liver transplantation
Christine Hwang1, Amal Aqul2, Yong Kwon1, Madhukar Patel1, Parsia Vagefi1, Malcolm MacConmara3.
1Surgery, UT Southwestern Medical Center, Dallas, TX, United States; 2Pediatrics, UT Southwestern Medical Center, Dallas, TX, United States; 3TransMedics, Andover, MA, United States
Introduction: Normothermic machine perfusion (NMP) is a method of organ preservation that is routinely used in adult transplantation. This technology is not yet commonly embraced in pediatric transplantation. We examined practice patterns of NMP use in pediatric liver transplantation.
Methods: The STARfile was queried to identify all pediatric patients, defined as those who were transplanted prior to the age of 18 years, who received a liver transplant between January 1, 2016 to December 31 2024. Those who were transplanted with a liver preserved with static cold storage (SCS) were compared to those transplanted with a liver preserved with NMP. Donor and recipient demographic data were examined, as were outcomes.
Results: There were 4226 pediatric livers transplanted during this period, of which 40 (0.95%) were preserved with NMP. The first livers preserved with NMP were transplanted in pediatric recipients in 2022 (n=2), and this has steadily increased through 2024 (n=25). The numbers of SCS and NMP livers transplanted over this time are shown in the figure; we see an overall decrease in the number of livers transplanted since 2016. The greatest number of livers preserved with SCS were procured in Region 3 (n=723), while the greatest number of livers preserved with NMP were procured in Region 5 (n=8). Recipient ages for SCS vs. NMP livers were 5.6 + 0.1 years vs. 8.2 + 1.1 years (p = NS); donor ages were 12.3 + 11.3 years vs. 19.4 + 10.5 years (p=NS); preservation times were 6.7 + 2.3 hours vs. 14.9 + 5.3 hours (p<0.05); and distance to transplant centers were 359.0 + 357.8 miles vs. 603.9 + 522.4 miles (p<0.05), respectively. Wait time for patients receiving a SCS liver was 144.8 + 287.5 days vs. 173.8 + 327.1 days in an NMP liver (p=NS). The average MELD/PELD score in the SCS group was 13 + 15, and in the NMP group, 18 + 15 (p<0.05). Use of technical variant grafts (TVG) were 30.25% in the SCS group, and 55.26% in the NMP group (p<0.05).
The most common diagnosis for recipients was biliary atresia, at 34.1% (14) of the cohort. Three centers accounted for 63.4% of NMP use, at 29.2% (12), 22.0% (9), and 12.2% (5). Three patients received multi-organ transplants, all of which were liver-kidney transplants. There were no donation after cardiac death (DCD) donors used in the recipients, but 8 DCD livers transplanted in the SCS group.
When examining outcomes, 85.75% of SCS patients were alive, vs. 94.12% of NMP patients. Death occurred in 8.56% of SCS patients and 2.94% of NMP patients; 4.07% of SCS and 2.94% of NMP patients were retransplanted.
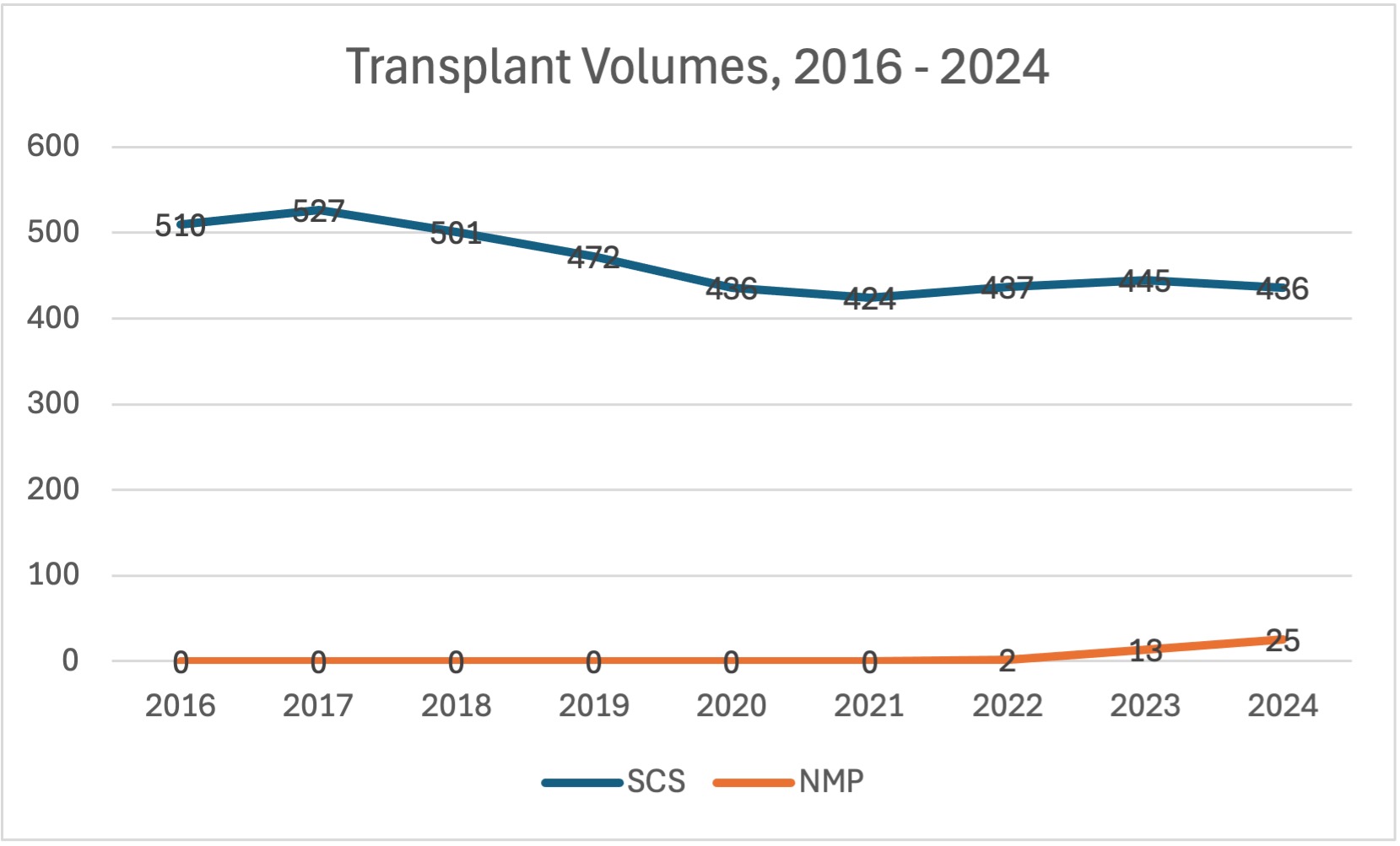
Conclusion: Use of NMP in pediatric liver transplantation has increased rapidly in the past two years. There appears to be potential to increase the number of livers transplanted with NMP use, especially with decreasing numbers of liver transplants. TVGs, which are used in the smallest patients where there is difficulty in finding a suitably sized organ, are significantly more transplanted in the NMP group. DCD livers also appear to be an untapped source to increase volume of livers transplanted into pediatric patients. It is interesting to see that although wait times are similar between the groups, NMP recipients were sicker based on MELD/PELD score. In an era of decreasing volume of pediatric transplants, NMP offers the opportunity to increase liver transplants with the opportunity to pursue TVG and DCD allografts.
References:
[1] Normothermic machine perfusion
[2] Transplantation
[3] Pediatric
[4] Liver
Lectures by Christine Hwang
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Thu-18 16:00 - 17:00 |
Best Liver Abstracts | Is Portable Normothermic Machine Perfusion the Way Forward for Widespread Adoption of Split Livers in the United States? | MOA 5 |
|
Sat-20 15:30 - 16:30 |
All about donors - education, assessment and management | Emergence of Normothermic Machine Perfusion in Pediatric Transplantation in the United States | MOA 4 |
|
Sun-21 07:00 - 07:50 |
Liver transplantation - expanding the donor pool | Practice Patterns of Normothermic Machine Perfusion Use in Pediatric Liver Transplantation | MOA 3 |
