Emergence of normothermic machine perfusion in pediatric transplantation in the United States
Christine Hwang1, Amal Aqul2, Yong Kwon1, Madhukar Patel1, Parsia Vagefi1, Malcolm MacConmara3.
1Surgery, UT Southwestern Medical Center, Dallas, TX, United States; 2Pediatrics, UT Southwestern Medical Center, Dallas, TX, United States; 3TransMedics, Andover, MA, United States
Introduction: Normothermic machine perfusion (NMP) has become commonplace in adult transplant practices where it has demonstrated enhanced utilization and improved outcomes for liver, heart and lung transplants. This technology is not used as frequently in pediatric transplantation. We examined practice patterns of utilization of NMP in pediatric transplantation in the United States.
Methods: Using the OPTN STARfile, 8797 pediatric recipients transplanted between January 1, 2015 and December 31, 2024 were identified. Patients transplanted with an organ preserved with NMP were analyzed. Donor, procurement and recipient data were examined, and outcomes were compared.
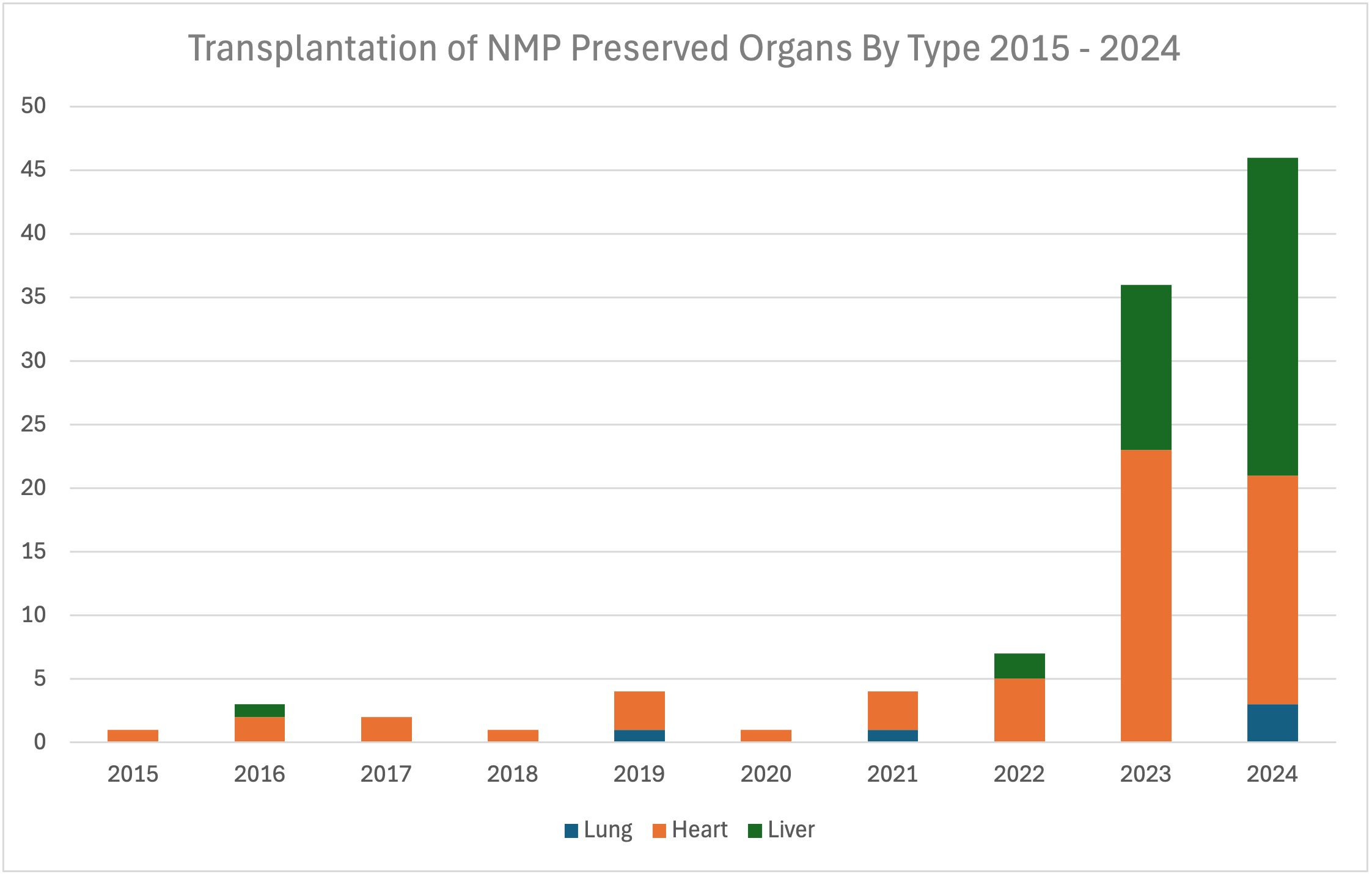
Results: Liver, heart, and lungs preserved with NMP have been used since 2015 in pediatric transplants. One hundred and four children received organs preserved using NMP, representing 1.2% of all pediatric transplants. Of those, there were 41 liver (0.9%), 58 (1.4%) heart, and 5 lung (1.2%) transplants. The first pediatric case was done using an NMP-preserved heart in 2015. Trends show steady increases in adoption with 46 organs transplanted in 2024.
NMP-preserved organs have generally been transplanted in older children, 8.2 ± 1.1 years (liver), 9.9 ± 5.8 years (heart), and 14.6 ± 2.1years (lung), using younger donors, 19.4 ± 10.5 years (liver), 15.3 ± 9.6 years (heart), and 17.8 ± 3.0 years (lung). Interestingly, an exception to this has recently been seen in young liver recipients receiving size-reduced or split livers after preservation using NMP. For all organs, NMP was associated with longer preservation times of 14.9 ± 5.3 hrs (liver), 4.4 ± 2.5 hrs (heart), and 8.8 ± 3.0 hrs (lung), with greater distances from donor to recipient, 604 ± 522 miles (liver), 466 ± 340 miles (heart), and 545 ± 222 miles (lung). There were no donation after cardiac death (DCD) donors transplanted in liver or lung, but 25% of hearts were from DCD donors.
One year graft survival was 92.6% (liver), 84.3% (heart), and 37.5% (lung). Death occurred in 2.70% of liver recipients, 14.0% of heart recipients, and 40.0% of lung recipients. Retransplantation occurred in 0 heart recipients, 2.70% liver recipients, and 20.0% lung recipients.
Conclusion: Use of NMP in pediatric transplantation has increased gradually over the past decade. Similar to adult practices, NMP is associated with wider logistic reach and more complex donor practices. At present, only heart transplantation has utilized DCD donors using NMP; however, the prospect to safely increase organ availability to all wait-listed children by carefully expanding use of all donor types is now within reach.
References:
[1] Pediatrics
[2] Organ Preservation
[3] Normothermic Machine Perfusion
[4] Liver
[5] Transplantation
[6] Lung
[7] Heart
Lectures by Christine Hwang
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Thu-18 16:00 - 17:00 |
Best Liver Abstracts | Is Portable Normothermic Machine Perfusion the Way Forward for Widespread Adoption of Split Livers in the United States? | MOA 5 |
|
Sat-20 15:30 - 16:30 |
All about donors - education, assessment and management | Emergence of Normothermic Machine Perfusion in Pediatric Transplantation in the United States | MOA 4 |
|
Sun-21 07:00 - 07:50 |
Liver transplantation - expanding the donor pool | Practice Patterns of Normothermic Machine Perfusion Use in Pediatric Liver Transplantation | MOA 3 |
