Elizabeth M Sonnenberg, United States
Assistant Professor
Transplant Surgery
University of Pennsylvania
The impact of revisions to the KDPI for pediatric kidney transplant candidates in the US and utilization of KDPI<35 kidneys in the contemporary era
Elizabeth Sonnenberg1,2,3, Sandra Amaral3,4,5, Siqi Zhang4, Jeremy Rubin6, Matthew H Levine1,2, Vishnu S. Potluri3,4,7.
1Department of Surgery, Hospital of the University of Pennsylvania, Philadelphia, PA, United States; 2Department of Surgery, Children's Hospital of Philadelphia, Philadelphia, PA, United States; 3Leonard Davis Institute of Health Economics, University of Pennsylvania, Philadelphia, PA, United States; 4Center for Clinical Epidemiology and Biostatistics, University of Pennsylvania Perelman School of Medicine, Philadelphia, PA, United States; 5Division of Nephrology, Department of Pediatrics, Children’s Hospital of Philadelphia, Philadelphia, Philadelphia, PA, United States; 6Department of Biostatistics, Epidemiology and Informatics, University of Pennsylvania Perelman School of Medicine, Philadelphia, PA, United States; 7Renal-Electrolyte and Hypertension Division, Department of Medicine, Hospital of the University of Pennsylvania, Philadelphia, PA, United States
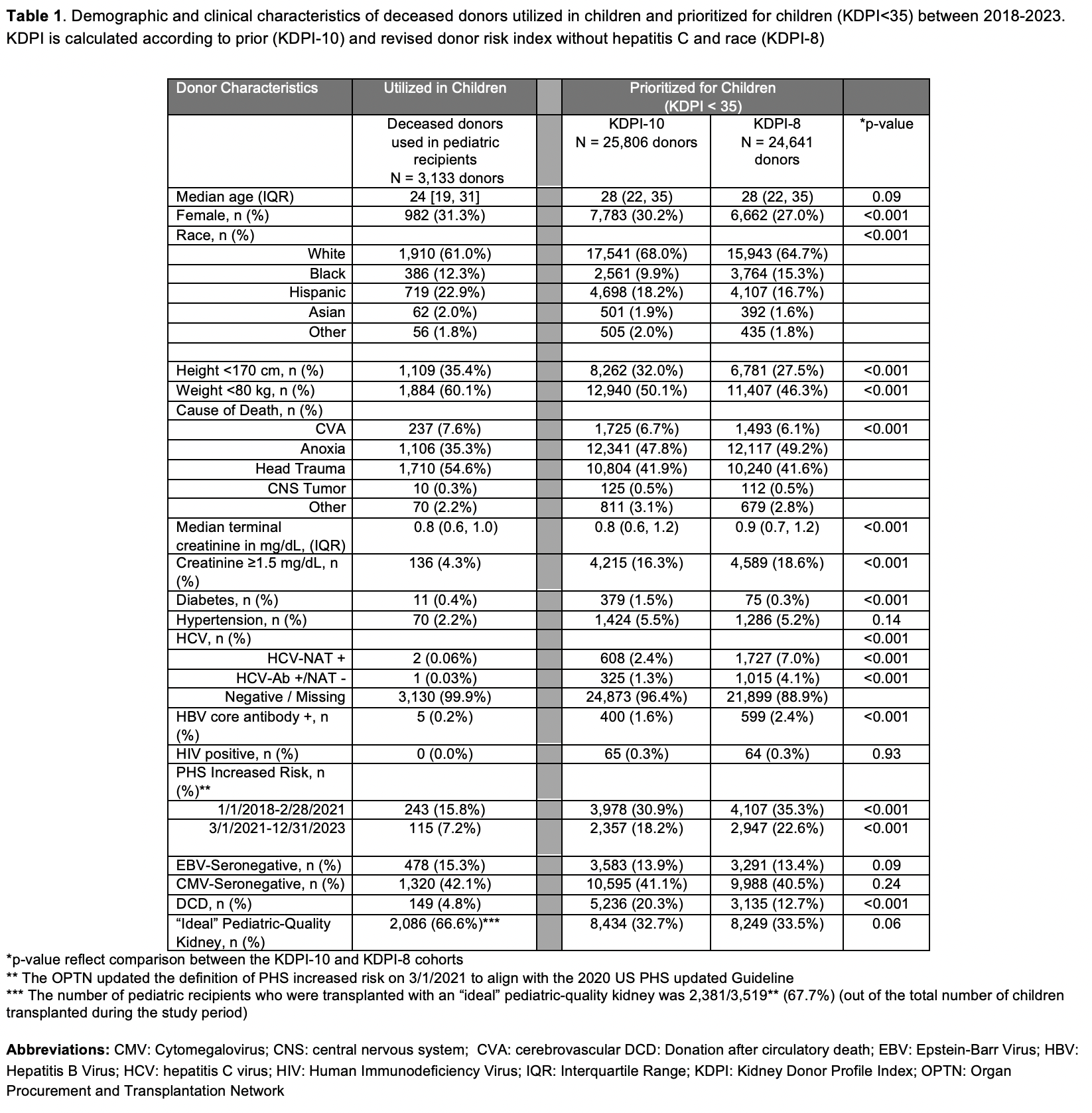
Introduction: In the US, children receive priority only for kidney donor profile index (KDPI) <35 kidneys. The KDPI is a composite measure of deceased donor kidney quality derived from donor variables and was intended to discriminate graft failure risk among adult recipients. Recently, the components and coefficients used to calculate the KDPI were changed. We sought to compare characteristics of deceased donors prioritized for pediatric candidates using the KDPI with 10 variables (KDPI-10) and the refit KDPI without hepatitis C virus (HCV) serostatus and race (KDPI-8). Secondarily, we sought to describe the allocation categories of recipients who receive these high-quality deceased donor kidneys since adult candidates with certain attributes supercede allocation to pediatric candidates.
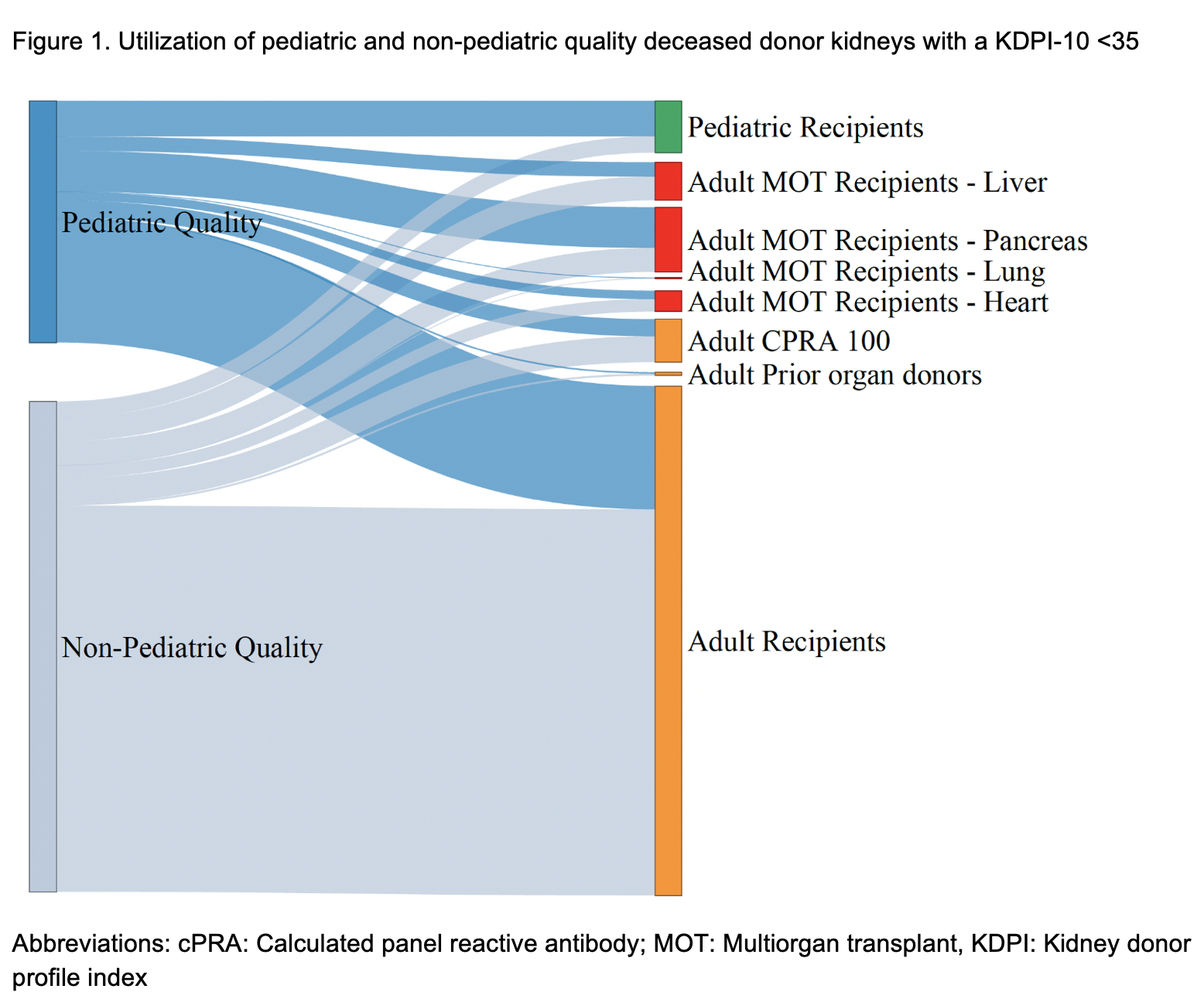
Methods: Using 2018-2023 Organ Procurement and Transplant Network (OPTN) data, we compared the characteristics of donors that would have been prioritized for pediatric candidates (i.e. KDPI<35) using KDPI-10 and KDPI-8 (new re-fit model). Since pediatric transplant providers often have different criteria beyond KDPI to optimize graft longevity and minimize risks, we categorized deceased donors as “ideal” pediatric-quality if: age <35 with brain death, without infectious risk, diabetes, hypertension, or creatinine ≥ 1.5mg/dL. We next retrospectively examined the utilization of all KDPI-10<35 kidneys and “ideal” pediatric-quality kidneys with KDPI-10<35 by recipient category. Recipient categories reflect the OPTN allocation schema order for candidates: 1) adult multiorgan transplant (MOT), 2) candidates with computed panel reactive antibody (cPRA) 100, 3) prior living donors, and then 4) children < 18 yrs of age at time of listing.
Results: Compared to the KDPI-10 cohort, the KDPI-8 cohort had more Black (15.3% vs 9.9%, p<0.001), HCV-seropositive donors (11.1% vs 3.7%, p<0.001), and fewer donors that donated after circulatory death (12.7% vs 20.3%, p<0.001)(Table 1). The overall proportion of KDPI<35 donors that would meet the definition of “ideal” pediatric-quality remained similar (32.7% KDPI-10 vs 33.5% KDPI-8, p=0.06). Among “ideal” pediatric-quality donors with a KDPI-10 <35, 34.9% of kidneys were allocated to adults in categories ahead of children and 14.4% of donors had both their kidneys preferentially allocated to adult recipients (Figure 2). Most of these kidneys (77.6%) were transplanted into MOT recipients. Furthermore,1,425 “ideal” pediatric-quality donors were classified with a KDPI-10≥35 over the study period and would not have been allocated to children based on this classification.
Conclusions: The change to KDPI-8 is unlikely to affect the proportion of “ideal” pediatric-quality kidneys with a KDPI<35. Yet, in the US, limitations in KDPI-based allocation and categorical preference for certain candidates impedes pediatric candidates’ access to the highest quality kidneys.
References:
[1] organ allocation
[2] kidney donor profile index