Elizabeth M Sonnenberg, United States
Assistant Professor
Transplant Surgery
University of Pennsylvania
Deceased donor organ allocation policy: An untapped opportunity to reduce the burden of EBV among pediatric kidney transplant recipients
Vishnu S. Potluri1,2,3, Sandra Amaral2,3,4, Siqi Zhang4, Chethan M Puttarajappa5, Elizabeth Sonnenberg2,6,7.
1Renal-Electrolyte and Hypertension Division, Department of Medicine, Hospital of the University of Pennsylvania, Philadelphia, PA, United States; 2Leonard Davis Institute of Health Economics, University of Pennsylvania, Philadelphia, PA, United States; 3Center for Clinical Epidemiology and Biostatistics, University of Pennsylvania Perelman School of Medicine, Philadelphia, PA, United States; 4Division of Nephrology, Department of Pediatrics, Children’s Hospital of Philadelphia, Philadelphia, Philadelphia, PA, United States; 5 Renal-Electrolyte and Hypertension Division, Department of Medicine, University of Pittsburgh, Pittsburgh, PA, United States; 6Department of Surgery, Hospital of the University of Pennsylvania, Philadelphia, PA, United States; 7Department of Surgery, Children's Hospital of Philadelphia, Philadelphia, PA, United States
Introduction: Latent Epstein-Barr Virus (EBV) infection varies by age, with about 50% of 6- to 8-year-olds and 10% of individuals over 18 years old being EBV-seronegative. For an EBV-seronegative recipient (EBV R-), the donor’s EBV serostatus (EBV D+ or D-) alters the risk of EBV DNAemia and post-transplant lymphoproliferative disorder (PTLD), with an EBV D+/R- pairing elevating the risk of both compared to EBV D-/R-. In the US, the National Organ Transplant Act (NOTA) directs the Organ Procurement and Transplantation Network (OPTN) to “recognize the differences in health and in organ transplantation issues between children and adults throughout the system and adopt criteria, policies, and procedures that address the unique health care needs of children”. This has translated into prioritizing children for kidney donor profile index (KDPI) <35 donors. Yet, despite the high prevalence of EBV-seronegativity among children, the current allocation system does not consider donor EBV serostatus when allocating kidneys to pediatric recipients. We sought to understand the utilization of EBV D- kidneys with a KDPI<35 in relation to the EBV serostatus of pediatric recipients.
Methods: Using 2018-2023 OPTN data we analyzed the clinical characteristics of deceased donors and pediatric recipients (age <18) by EBV serostatus. We analyzed the proportion of EBV seronegative recipients who received an EBV D- kidney and the utilization of all EBV D- kidneys with a KDPI <35.
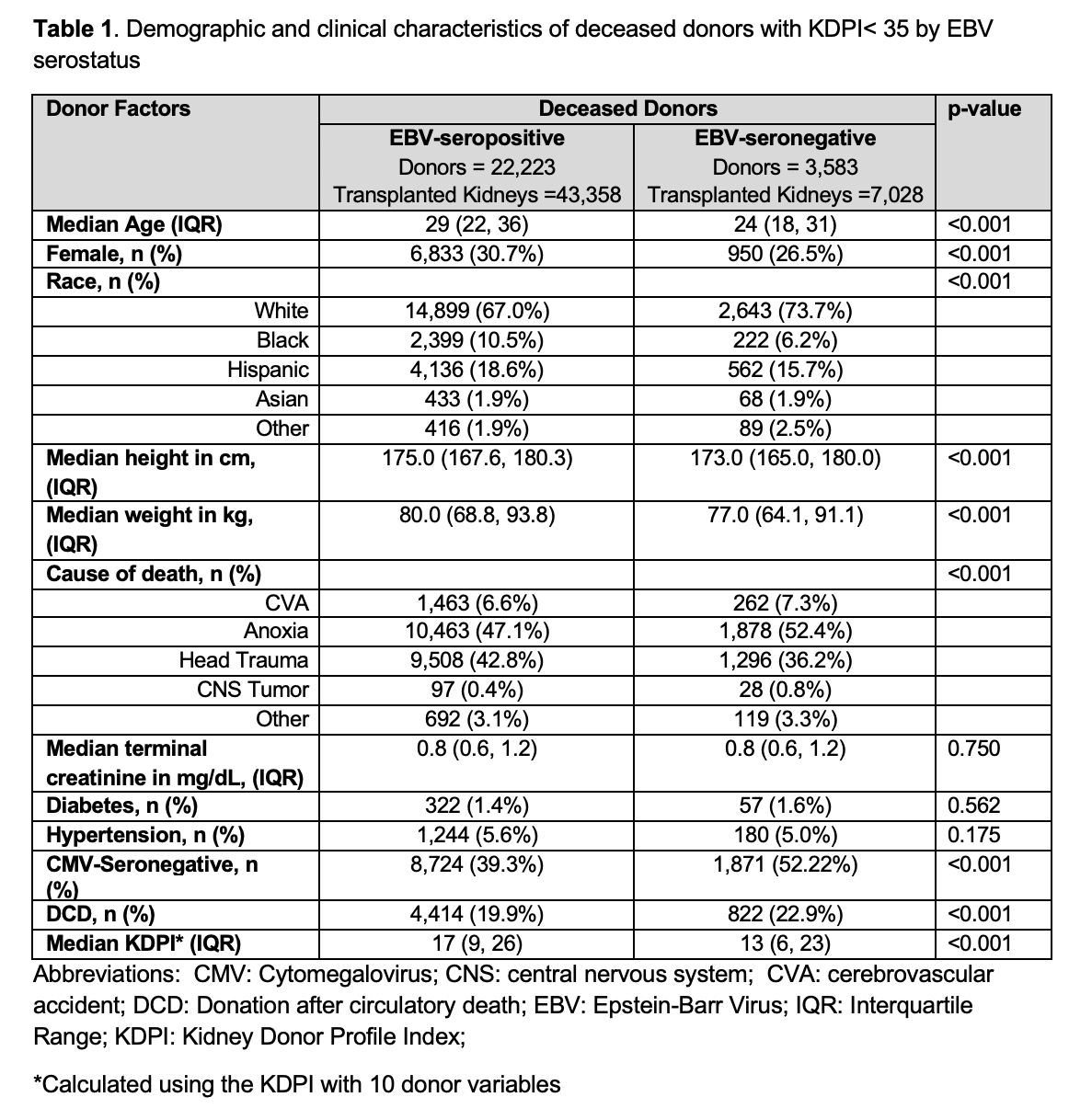
Results: Among the 25,806 donors, 13.9% were EBV D- and these donors were younger (median age 24 vs. 29, p-value <0.001) with a lower median KDPI (13 vs. 17, p-value<0.001) than EBV D+ donors (Table 1). Among the 3,380 pediatric recipients, 41.6% were EBV R-, and they were younger (median age 10 vs 14, p-value <0.001) and more likely to be White (45.9% vs. 29.0%, p-value <0.001) than EBV R+ recipients. Only 15.4% of EBV R- recipients received an EBV D-/R- transplant (n=217, representing just 3.1% of all EBV-D- kidneys) while 84.6% (n=1,191) received an EBV D+/R- transplant. For the EBV D- kidneys with a KDPI <35, 25.0% were transplanted into adults with higher priority than children, 4.5% were transplanted into EBV-seropositive pediatric recipients, and 67.0% were transplanted into adults (Figure 1). A total of 1,419 EBV-D- kidneys from pediatric donors had a KDPI ≥ 35 and therefore were not prioritized for children.
Conclusions: Most children who are EBV-seronegative receive a deceased donor organ that confers the highest risk of developing EBV DNAemia and PTLD. Yet, there are more donors with a KDPI<35 that are EBV-seronegative than pediatric EBV-seronegative recipients. Policies that facilitate prioritizing EBV-seronegative children for EBV-seronegative donors should be considered to minimize the morbidity, mortality, and health care utilization associated with EBV-associated diseases and abide by NOTA’s directive to recognize the unique health needs of children.
" href="https://app.ipta2025.org/papers/body/386#">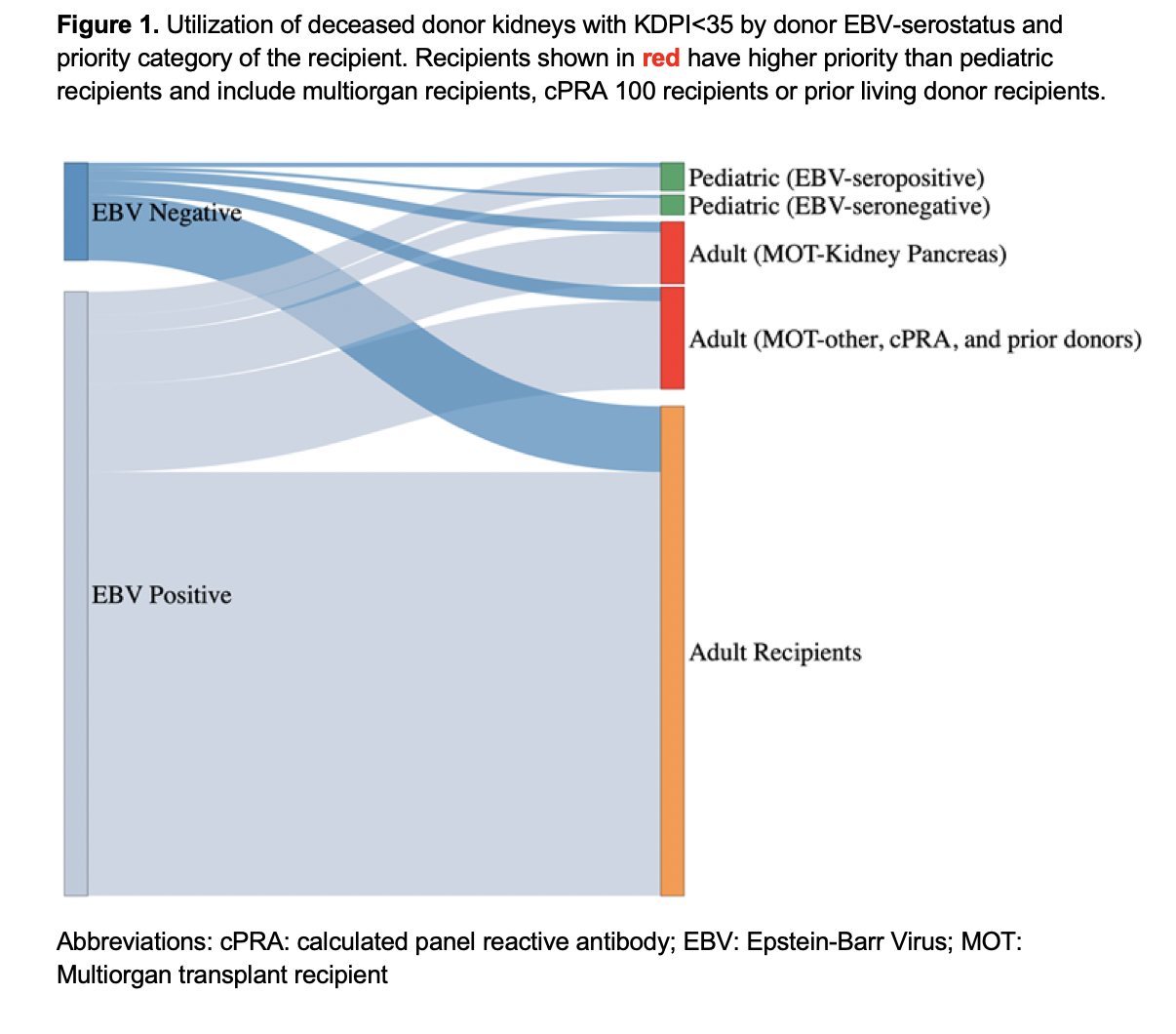
References:
[1] Epstein-Barr Virus
[2] organ allocation
[3] post-transplant lymphoproliferative disorder
[4] kidney transplant
