The impact of living donor age and sex on pediatric kidney transplant outcomes
Stella Kilduff1,2, Jiafeng Li4, Carlos Becerril-Romero1,2, Bridget Whitehead3, Debora Matossian1,2, Priya S Verghese1,2.
1Pediatric Nephrology, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; 2Pediatrics, Northwestern University Feinberg School of Medicine, Chicago, IL, United States; 3Gastroenterology, Hepatology, and Nutrition, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; 4Stanley Manne Children’s Research Institute, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States
Introduction: Optimizing kidney transplant (KTx) longevity is crucial for addressing organ shortages and reducing the number of transplants children with kidney failure need in their lifetime. Most research focuses on adults and deceased donors, leaving gaps in pediatric living donor transplants. This study aims to examine how donor-recipient sex mismatch impacts outcomes to enhance donor selection.
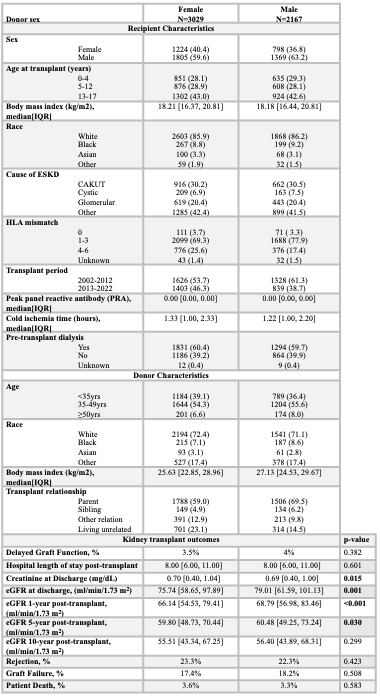
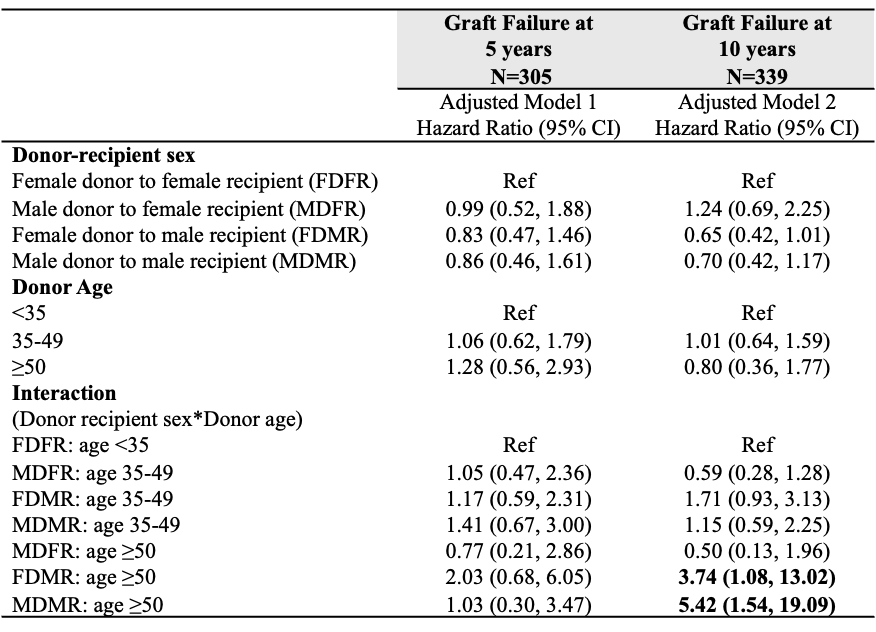
Methods: We conducted a retrospective study of pediatric recipients (<18 years) who received living donor KTx from 01/01/02 to 12/31/22, using the Scientific Registry of Transplant Recipients (SRTR) and excluding multi-organ transplants. Descriptive statistics were used to report baseline characteristics and outcomes by donor sex. Multivariate Cox models analyzed the impact of donor-recipient sex [Female donor to female recipient (FDFR), Male donor to female recipient (MDFR), Female donor to male recipient (FDMR), and Male donor to male recipient (MDMR)] on 5- and 10-year death censored graft failure (DCGF), adjusted for race/ethnicity, recipient age, cause of ESKD, pre-transplant dialysis, HLA mismatch, transplant period (2002-2012 vs. 2013-2022), and donor age (<35, 35-49, ≥50).
Results: A total of 5,196 recipients had a median follow up time of 7.3 years. There were 1,224 (23.6%) FDFR, 798 (15.4%) MDFR, 1,805 (34.7%) FDMR, and 1,369 (26.3%) MDMR. Most donors were 35-49 years old, and recipients were 13-17 years, with parents as the most common donor relationship (Table 1). Recipients of male donors had higher eGFR at discharge, 1-, 5-, and 10-years post-transplant but this was only statistically significant at discharge. Further, no significant differences were found in rejection, graft failure, or DCGF based on donor sex. In the multivariable Cox proportional hazards model, the interactions between donor age ≥50 with FDMR (HR: 3.74, 95% CI: 1.08, 13.02) and MDMR (HR:5.42, 95% CI: 1.54, 19.09) significantly predicted DCGF at 10-years when compared to (Table 2). This effect was not seen at 5-year graft survival.
Conclusion: Male donor recipients had higher eGFR but no significant differences in rejection or graft survival. Interactions between donor age ≥50 and recipient sex showed the highest 10-year DCGF risk in male recipients, especially with male donors, indicating that older male donors may lead to worse survival in male recipients.
Siragusa Transplant Center Research and Innovation Grant.
[1] Pediatric Kidney Transplant
[2] Donor-Recipient Sex Mismatch
[3] Allograft Survival
[4] Living Donor Transplant
[5] Donor Age