Pubertal stage specific changes in T-cell subpopulations in healthy individuals and pediatric kidney transplant recipients
Harm H Boer1,2, Huib H Jong1,2, Femke F.H.M. Vrieling-Prince1,2, Michiel M.H.G. Betjes3, Antonia A.H.M. Bouts4, Marlies E.A.M. Cornelissen5, Edmond E.H.H.M. Rings7, Kim K.C. Heezen6, Ton A.W. Langerak6.
1Pediatric Nefrology, Erasmus MC- Sophia's children's hospital, Rotterdam, Netherlands; 2Transplant Institute, Erasmus MC, Rotterdam, Netherlands; 3Nephrology, Erasmus MC, Rotterdam, Netherlands; 4Pediatric Nefrology, Amsterdam UMC- Emma Children’s Hospital, Amsterdam, Netherlands; 5Pediatric Nefrology, Radboudumc- Amalia Children’s Hospital, Nijmegen, Netherlands; 6Medical immunology, Erasmus MC, Rotterdam, Netherlands; 7Pediatrics, Erasmus MC- Sophia's children's hospital, Rotterdam, Netherlands
Background: During adolescence an increase in early graft loss is observed in pediatric kidney transplant(KTx) recipients in comparison to other periods in life, regardless of therapy compliance. Given the importance of T-cell activity in renal graft rejection, we hypothesize that pubertal hormonal changes shift the immune system towards a more pro-inflammatory phenotype. In a step towards this hypothesis, this study explored the changes in T-cell subpopulations during puberty in healthy individuals and KTx-recipients.
Methods: Healthy individuals, median age 17 years(range: 8-29),and KTx-recipients, at least 1 year post transplantation, median age 16.5 years(range:7 to 30), were included in this multi-center, observational study. Pubertal maturation was assessed by subdividing participants into four different puberty stages(prepuberty, early, late, and post puberty), using skeletal age and Tanner stage. Peripheral blood samples were used to determine multiple differentiation stages of CD4, CD8, and Tcr-γδ Tcells subpopulations, using 8-color flow cytometry.
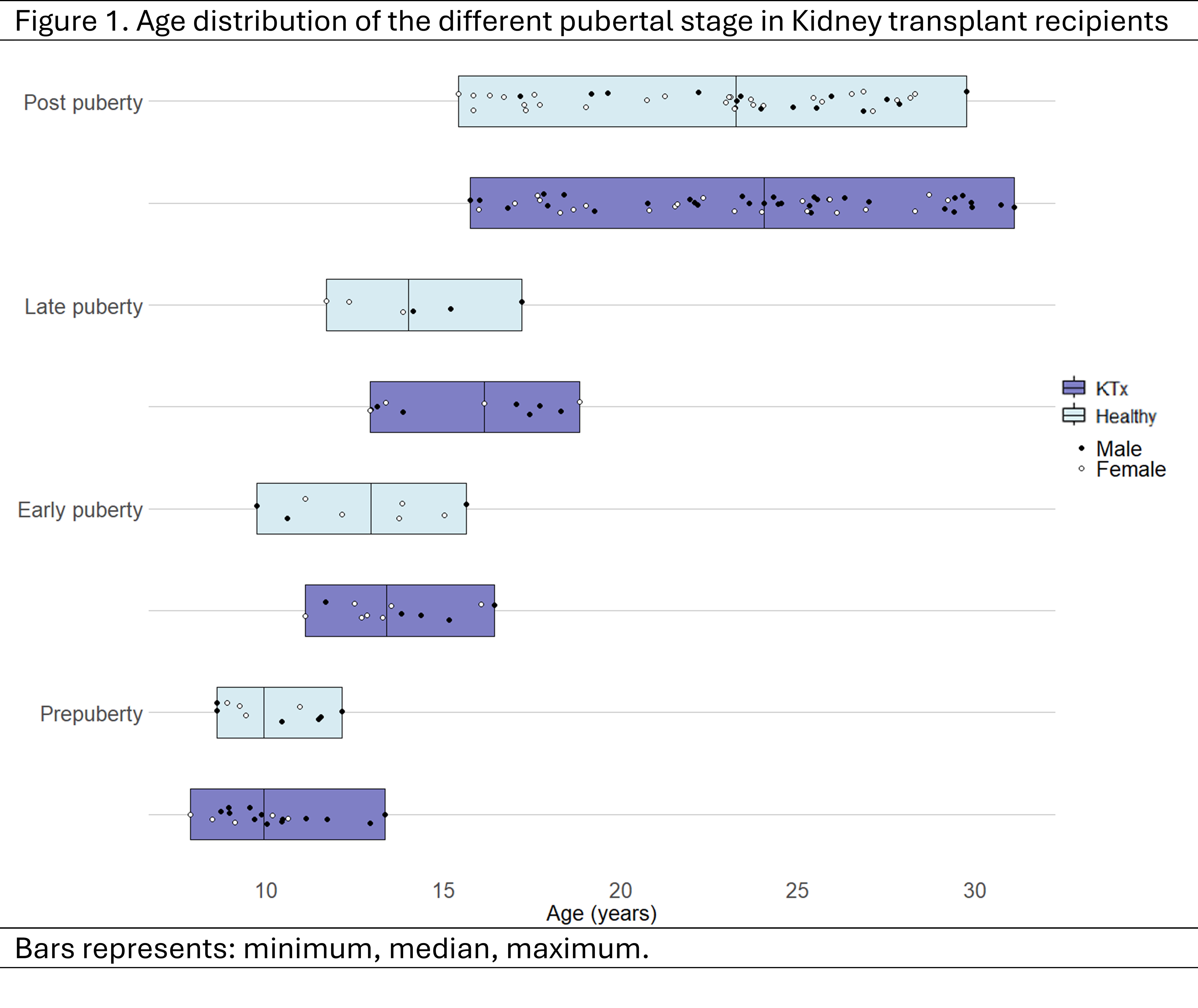
Results: In 66 healthy individuals (42% male, pre-: n=10, early-: n=8, late-: n=6, and postpubertal: n=42)were included. The range of age of the pubertal stages overlapped, as can be seen in Figure 1.
Absolute naïve CD4 T-cell and recent thymic emigrant(RTE) CD4 T-cell counts decreased over the course of puberty(p=0.014, p=0.021), while absolute CD4 effector memory cell counts increased(p=0.008). In post-hoc analysis, higher absolute cell counts were observed during early puberty compared to post puberty in CD4 RTE (Figure 2) and naïve T-cells, and Tcr-γδ Vδ1 T-cells (p=0.013, p=0.013, p= 0.037).
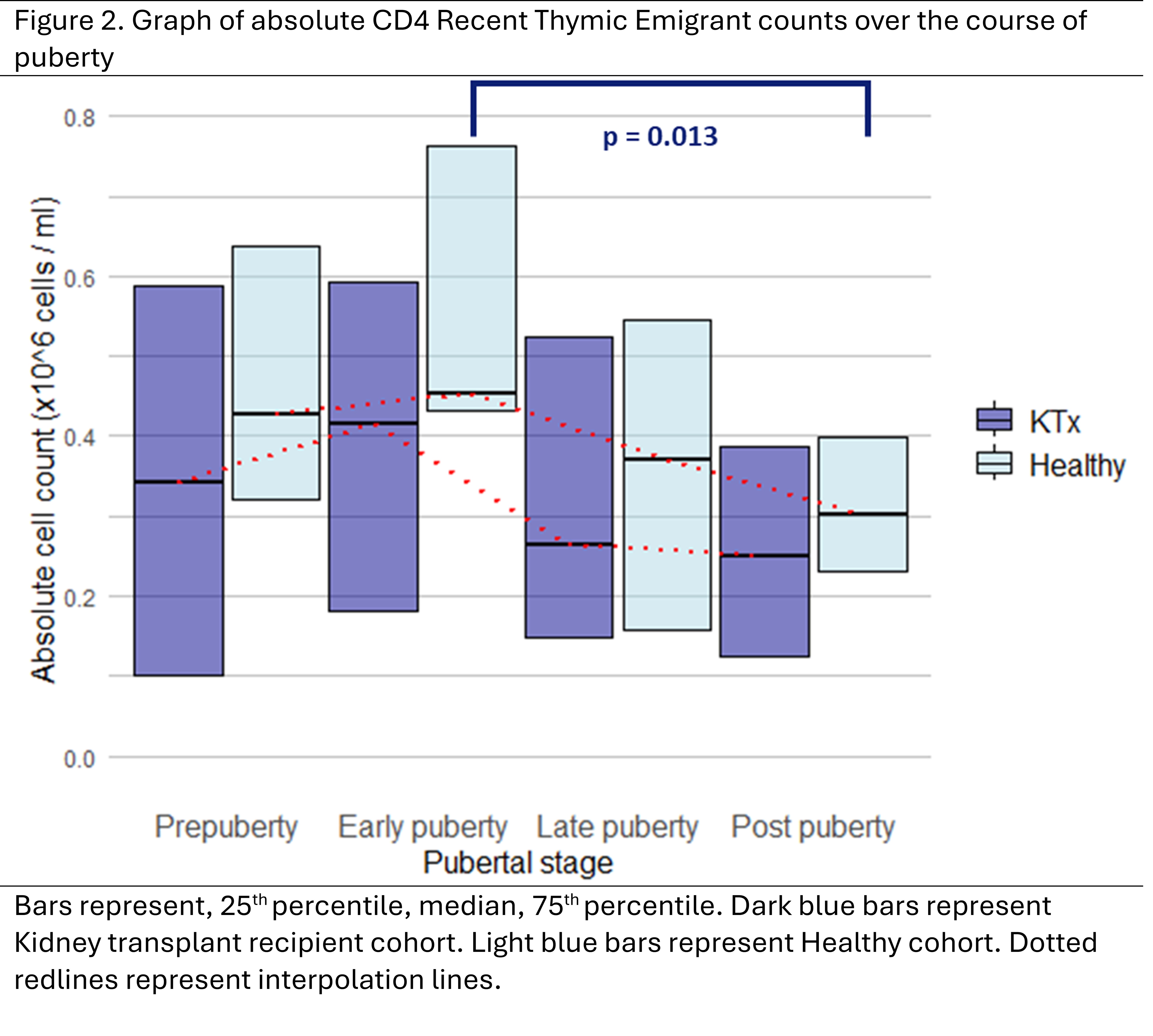
In 99 KTx-recipients(61% male, pre-: n= 19, early-: n=12, late-: n=12, and postpubertal: n=56) similar patterns were observed. Absolute CD4 naïve, and CD8 naïve T-cell counts decreased over the course of puberty(p=0.022, p=0.02), with post-hoc analysis observing a significant difference between pre-puberty and post-puberty(p=0.021, p=0.046). In RTE Tcr-γδ T-cell, absolute counts decreased during puberty(p=0.006), with post-hoc testing revealing a difference between pre-puberty and post-puberty (p=0.007).
Conclusion: Healthy individuals and KTx-recipients demonstrate a similar shift from a less mature to a more experienced and active immune profile over the course of puberty.