Guang-Peng Zhou, People's Republic of China has been granted the TTS Congress Scientific Awards

Guang-Peng Zhou, M.D.
Liver Transplantation Center, National Clinical Research Center for Digestive Diseases, Beijing Friendship Hospital, Capital Medical University, Beijing, China;
Clinical Center for Pediatric Liver Transplantation, Capital Medical University, Beijing, China;
Laboratory for Clinical Medicine, Capital Medical University, Beijing, China;
State Key Laboratory of Digestive Health, Beijing, China.
Email: guangpeng_zhou@ccmu.edu.cn
Dr. Guang-Peng Zhou is a surgical resident at the Liver Transplantation Center of Beijing Friendship Hospital, Capital Medical University. Since 2015, he has been under the tutelage of Professor Zhi-Jun Zhu, a famous liver transplant surgeon in mainland China, and has participated in over 300 cases of liver transplantation. Under the leadership of Prof. Zhi-Jun Zhu, their team completed the first case of cross-auxiliary double domino donor liver transplantation in 2013 and the first case of cross-auxiliary domino liver transplantation by exchange of partial liver between two patients with hypermethioninemia and OTCD in 2018. "Liver transplantation without donation" can be achieved by this way. He is currently engaged in clinical and basic research related to liver transplantation and hepatocyte transplantation for the treatment of inherited metabolic liver diseases. He has published several scientific research papers in international journals as the first or co-first author and participated in international conferences including TTS, IPTA and ILTS as oral or poster abstract presenter for several times. He obtained “Young Investigator Awards” in 2022 Joint International Congress of ILTS, ELITA, & LICAGE.
First single-center experience of minimally invasive pediatric living donor liver transplantation in China
Guang-Peng Zhou1,2,4,5, Zhi-Jun Zhu1,2,4,5, Lin Wei1,2,4,5, Zhi-Gui Zeng1,2,4,5, Wei Qu1,2,4,5, Li-Ying Sun3,4,5, Yu-Le Tan1,2,4,5, Jun Wang1,2,4,5.
1Liver Transplantation Center, Beijing Friendship Hospital, Capital Medical University, Beijing, People's Republic of China; 2National Clinical Research Center for Digestive Diseases, Beijing Friendship Hospital, Capital Medical University, Beijing, People's Republic of China; 3Department of Critical Liver Diseases, Liver Research Center, Beijing Friendship Hospital, Capital Medical University, Beijing, People's Republic of China; 4Clinical Center for Pediatric Liver Transplantation, Capital Medical University, Beijing, People's Republic of China; 5State Key Lab of Digestive Health, Beijing Friendship Hospital, Capital Medical University, Beijing, People's Republic of China
Introduction: The use of laparoscopic procedures for liver transplantation (LT) remains controversial. This study aimed to present our preliminary experience with a minimally invasive pediatric living donor liver transplantation (LDLT).
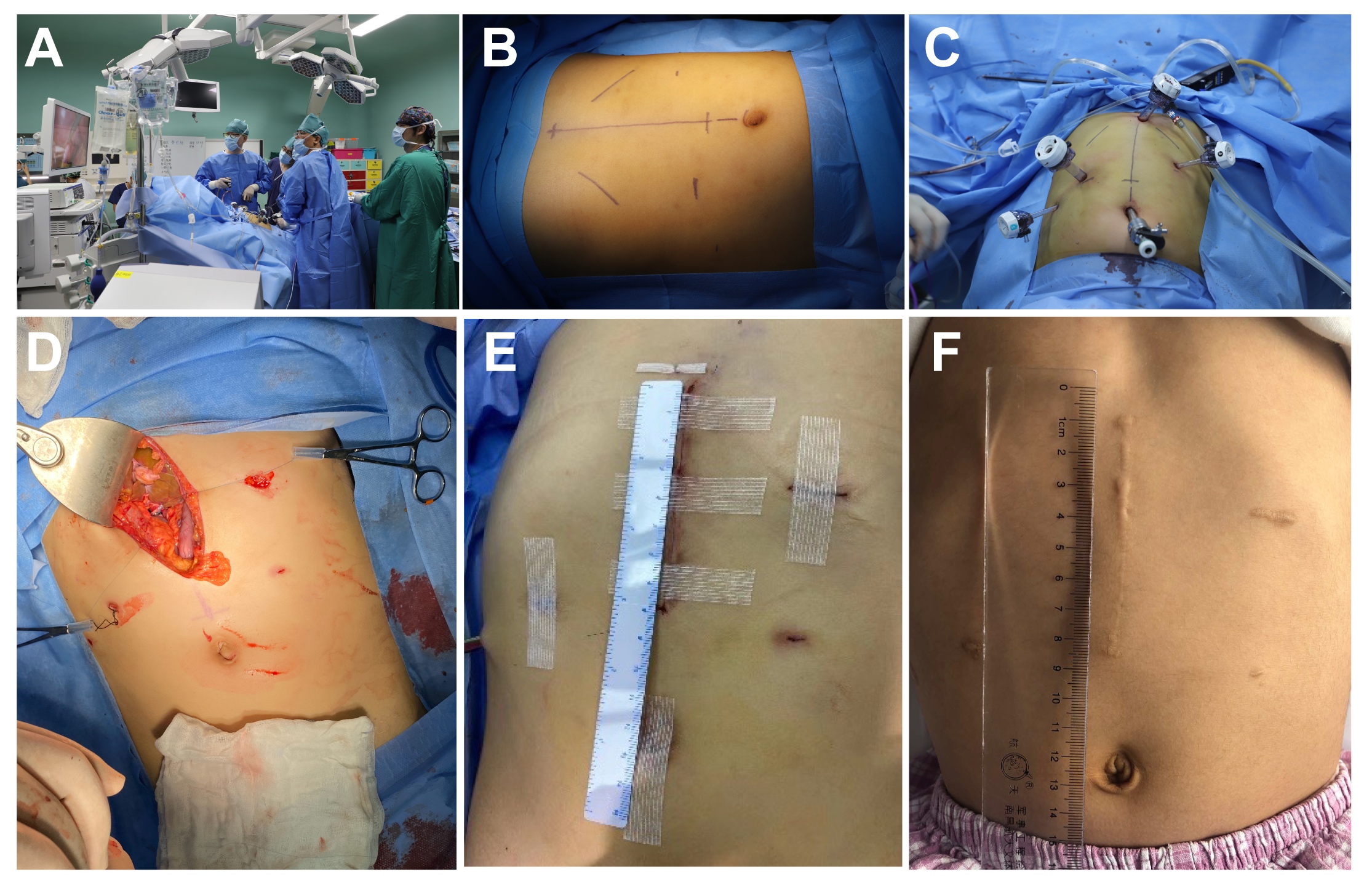
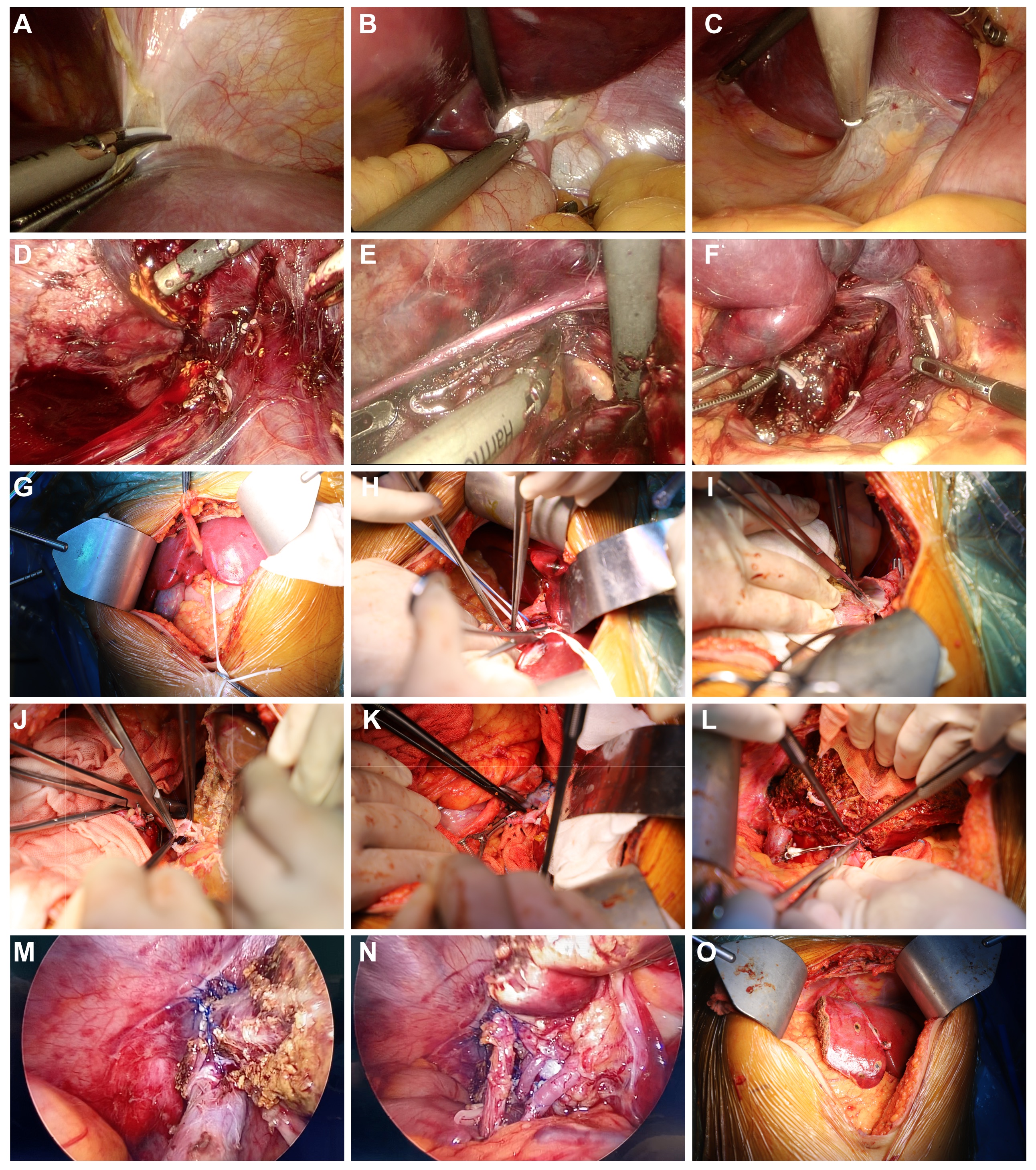
Methods: The medical records of pediatric patients who underwent laparoscopy-assisted LDLT, namely laparoscopic mobilization of the diseased liver followed by open explant hepatectomy and graft implantation using an upper midline incision at Beijing Friendship Hospital between November 2019 and March 2023, were retrospectively reviewed, focusing on demographics and pre-, intra-, and postoperative outcomes.
Results: Laparoscopy-assisted LDLT was successfully performed in all 13 pediatric patients. The mean total operative time was 478 min (range, 315-615 minutes), the median portal vein clamping time was 47 min (range, 33-107 minutes), the average time required to remove the liver was 229 min (range, 115-357 minutes), and the median cold ischemia time was 85 min (range, 29-214 minutes). The intraoperative course for all the recipients was uneventful. All patients recovered well without any significant acute postoperative problems, with only one patient presenting with hepatic artery thrombosis on postoperative day 1 who made a good recover after immediate thrombectomy and re-anastomosis. During a median follow-up of 41.8 (range, 24.3–64.3 months), all recipients survived with 100% graft survival.
Conclusion: This is the world's largest single-center cohort study of pediatric laparoscopy-assisted LDLT using an upper midline incision. Our results provide preliminary evidence for the safety and feasibility of minimally invasive LDLT in selected pediatric patients, which may be a reasonably compromised strategy before attempting pure laparoscopic LT.
Capital's Funds for Health Improvement and Research (No.2024-1-2022, No.2024-4-1111), Tongzhou District Health Development Project (KJ2024CX032), and Beijing Municipal Science & Technology Commission (No. Z211100002921026).
[1] Laparoscopy
[2] Minimally invasive surgery
[3] Liver transplantation
[4] Living donor liver transplantation
[5] Upper midline incision