Weihao Li, Netherlands has been granted the CareDx Congress Scientific Awards

Incidence and high-risk groups of hepatic artery thrombosis and stenosis after pediatric liver transplantation: Preliminary results from a retrospective, observational, multicentric study
Weihao Li1, Reinoud P.H. Bokkers1, Rene Scheenstra2, Rudi A.J.O. Dierckx3, Hermien Hartog4, Hubert P.J. van der Doef2.
1Department of Radiology, Medical Imaging Centre, University Medical Centre Groningen, Groningen, Netherlands; 2Division of Paediatric Gastroenterology and Hepatology, Department of Paediatrics, University Medical Centre Groningen, Groningen, Netherlands; 3Department of Nuclear Medicine and Molecular Imaging, Medical Imaging Center, University Medical Center Groningen, Groningen, Netherlands; 4Department of Surgery, Section of Hepatobiliary Surgery & Liver Transplantation, University Medical Center Groningen, Groningen, Netherlands
HEPATIC Registry.
Background: Hepatic artery complications (HACs) such as thrombosis (HAT) and stenosis (HAS) cause significant morbidity and mortality after pediatric liver transplantation (pLT); however, their incidence and risk factors remain poorly defined. This study aimed to investigate the incidence of HACs after pLT and identify high-risk groups.
Methods: We performed a retrospective, multicentric study from the HEPatic Artery stenosis and Thrombosis after liver transplantation In Children registry, which includes pLTs from 24 centers across 20 countries and six continents over a 20-year period. We examined the onset of HACs after pLT and analyzed the incidence of HACs across subgroups defined by pLT indication, age at pLT, donor type, transplant era, and annual center volume.
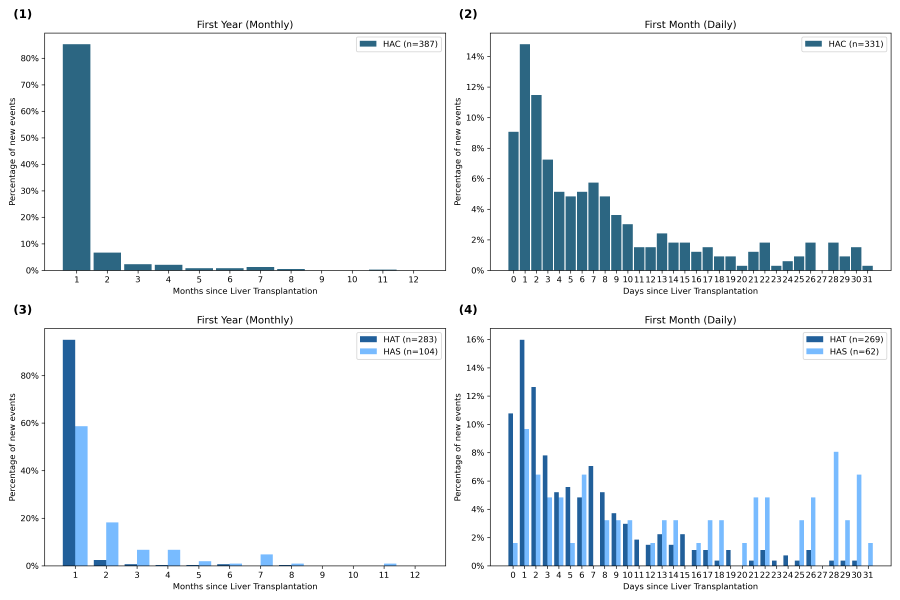
Results: A total of 8,469 pLTs were identified with 406 HACs, yielding an overall incidence of 4.8% (HAT: 3.4%; HAS: 1.4%). HACs occurred predominantly within the first month post-pLT (85.3%), with HAT peaking in the first week and HAS evenly distributed throughout the month. HAC incidence was higher after re-transplantation (6.5%) compared to primary pLTs (4.7%, p = 0.04) and after deceased donor liver transplantation (DDLT) compared to living donor liver transplantation (LDLT) (6.2% vs. 3.4%, p < 0.01). Among biliary atresia (BA) patients under 1 year, HAC rates were higher following DDLT than LDLT (7.6% vs. 3.2%, p < 0.01) and higher with whole grafts compared to partial grafts in DDLT (12.2% vs. 5.9%, p < 0.01). HAC rates significantly increased over time, from 3.6% (2002–2012) to 5.5% (2012–2022), and were highest in low-volume centers (11%, p < 0.01).
Conclusions: The overall incidence of HACs was 4.8%. Higher HAC incidence was observed in re-transplantations, DDLT (particularly with whole grafts in BA patients under 1 year), recent decade (2012–2022), and low-volume centers. Identifying these high-risk groups can help guide improvements in the prevention, detection, and management of HACs after pLT.
[1] hepatic artery complications
[2] pediatric liver transplantation
[3] incidence
[4] risk factor