
Thrombotic and hemorrhagic events after pediatric kidney transplantation: A single-center assessment of anticoagulation protocol
Javier Morelos-Zaragoza1, Amane Lachkar1, Djamel Elaribi1, Elodie Cheyssac1, Véronique Baudouin1, Charlotte Duneton1, Julien Hogan1.
1Pediatric Nephrology, Robert Debré Hospital, Paris, France
Aims/Purpose: Vascular thrombosis is a major complication of pediatric kidney transplantation, leading to graft loss and sensitization that may compromise future transplants. Prophylactic anticoagulation or antiplatelet therapy is commonly used; however, there is no consensus on indications or protocols, resulting in wide practice variability. Pediatric data remain limited, making anticoagulation management challenging due to balancing thrombotic and hemorrhagic risks. In 2013, our pediatric nephrology department revised its anticoagulation protocol to a more intensive approach. This study aims to assess clinical outcomes, focusing on thrombotic and hemorrhagic complications, and to examine their association with anticoagulation dosing and monitoring.
Methods: We retrospectively included all pediatric kidney transplant recipients from January 1, 2013, to December 31, 2022, at Robert Debré Hospital. Data collected included thrombotic and hemorrhagic complications and detailed anticoagulation management (Enoxaparin dosing and anti-Xa levels during the first week).
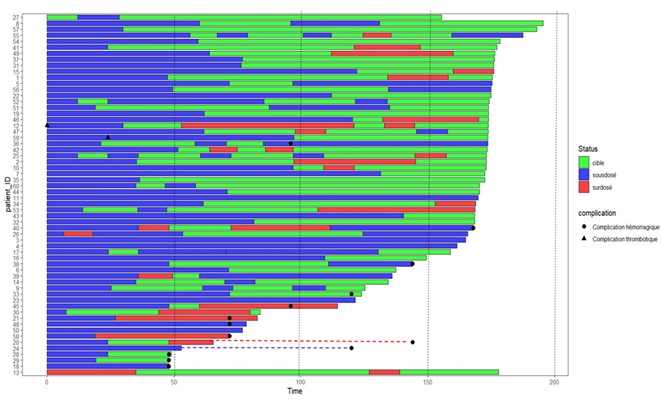
Results: We included 175 patients, of whom 99 (56.5%) received prophylactic anticoagulation due to thrombotic risk factors (donor/recipient weight <20 kg, multiple vessels, or prothrombotic conditions). Fourteen thrombotic events were observed (6/99 [6.1%] anticoagulated vs. 8/76 [10.5%] non-anticoagulated, p=ns). Graft loss occurred more frequently in the non-anticoagulated group (7/76 [9.2%]) compared to the anticoagulated group (1/99 [1%]). Hemorrhagic events were reported in 34 patients, with anticoagulation, male sex, and older age identified as independent risk factors. The median time to reach target anti-Xa (0.4–0.6 IU/mL) was 59.7 hours, with a median Enoxaparin dose of 70.5 IU/kg/12h. Male sex and younger age were associated with a longer time to target anti-Xa. Most bleeding events occurred at or below target anti-Xa levels (Figure 1).
Conclusion: Anticoagulation reduced thrombotic risk in high-risk patients but was associated with significant hemorrhagic complications. The current protocol results in delayed therapeutic anticoagulation and bleeding without apparent overdose. These findings support protocol modifications aimed at improving early thrombosis prevention in all patients while reducing hemorrhagic risks post-transplant.
[1] Graft thrombosis
[2] anticoagulation
[3] kidney transplantation