Impact of Epstein Barr Virus (EBV) status of lesions, 2016 WHO histologic grade and time of onset on outcome of Post-Transplant Lymphoproliferative Disorder (PTLD) in pediatric solid organ transplant (SOT) and hematopoietic stem cell transplant (HCT) recipients: Results of a prospective/retrospective multicenter study
Michael Green1, Lianna J Marks2, Mansi Agarwal3, Charles W Goss3, Vikas R Dharnidharka4.
1Pediatrics and Surgery , UPMC Children's Hospital of Pittsburgh , Pittsburgh , PA, United States; 2Pediatrics, Stanford University School of Medicine, Palo Alto, CA, United States; 3Biostatistics, Washington University School of Medicine, St. Louis , MO, United States; 4Pediatrics, Robert Wood Johnson Medical School at Rutgers University, New Brunswick, NJ, United States
the PTLD-MSMS group.
PTLD is an important cause of morbidity & mortality in pediatric SOT & HCT recipients. The goal of this study was to analyze the potential impact of EBV tumor status, WHO classification & timing of presentation on PTLD outcomes.
Methods: As part of a NIH funded, multi-center study of viral genomes in PTLD, we retrospectively & prospectively collected clinical data (demographics, transplant & PTLD characteristics, treatment, patient & graft survival) from adult & pediatric patients with biopsy-proven PTLD from 3 large USA transplant (Tx) centers. Participants < 18 years of age at the time of their Tx were included in this analysis. Time-to-event outcomes (time to death & time to death, organ loss or 2nd PTLD) were analyzed focusing on the impact of EBV tumor status, classification based on the 2016 WHO criteria (non-destructive vs destructive (polymorphic/ monomorphic) PTLD) & timing of presentation (early (< 12 mo) vs late (> 12 mo post-Tx)) using Kaplan-Meier methods. Multivariable modeling predicting 1-year mortality included age at Tx, WHO classification, time of presentation, Tx organ, & tumor EBV status was performed.
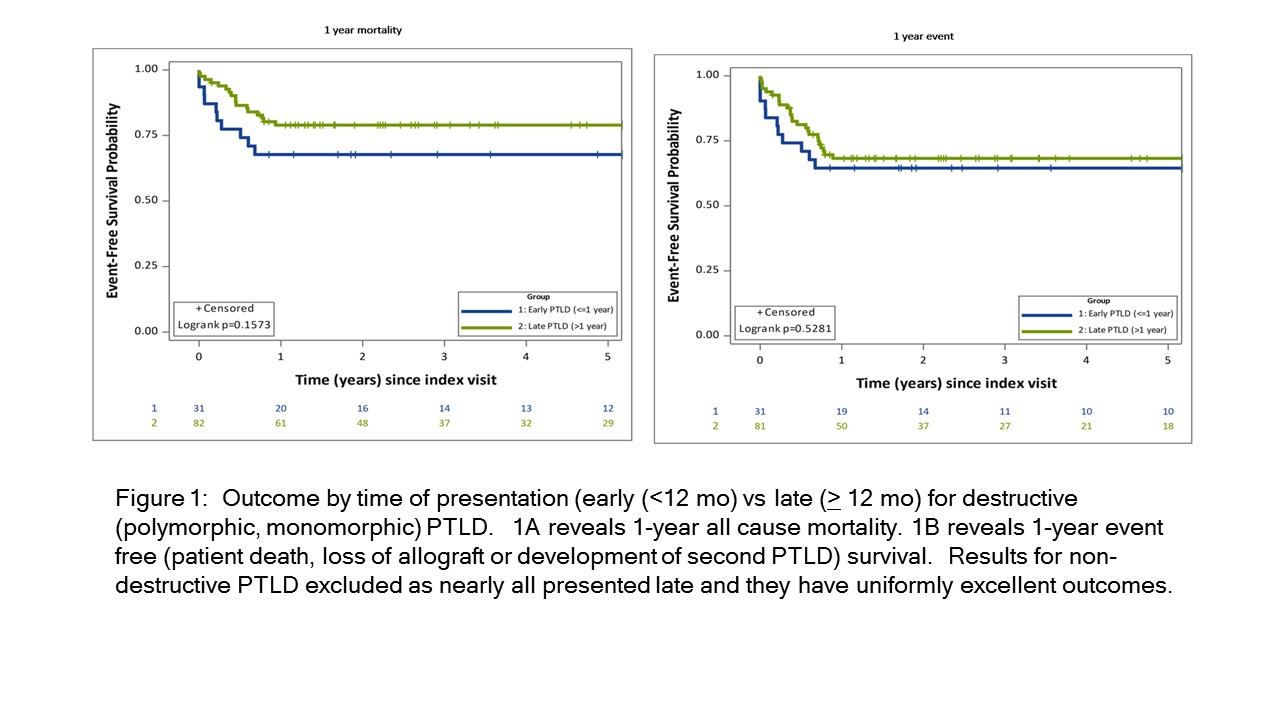
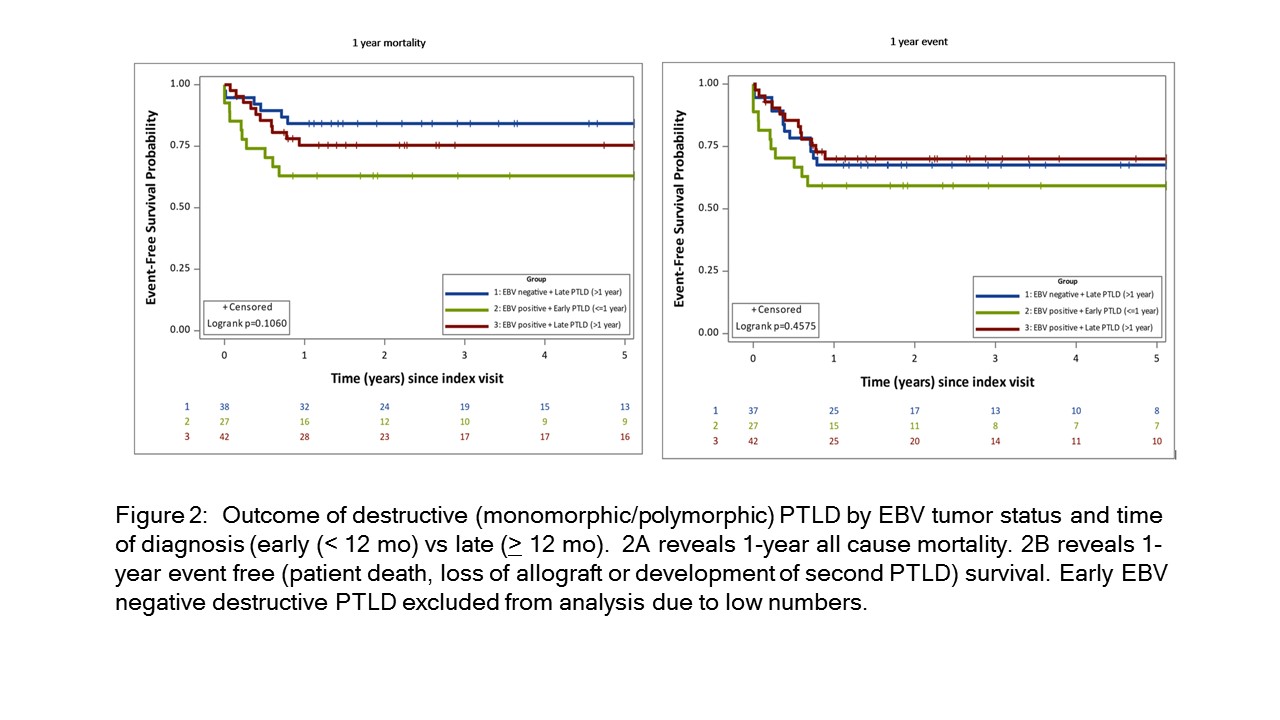
Results: 137 children diagnosed with PTLD were enrolled including recipients of heart (n=48), lung (n=25), liver (n-23), kidneys (n=17), HCT (n=6), intestine (n=5), multiple organs (n=12) & unknown (n=1). 31 children had early PTLD (27 EBV+ & 4 EBV-) while 104 had late PTLD (66 EBV+ & 38 EBV-). Overall 1-year patient & event-free (EF) survival were 80.3 (95% CI 72.8-86.1%) & 71.5% (95% CI 63.5-78.4%), respectively. Almost all nondestructive lesions presented late & had excellent outcomes; they were excluded from subsequent analyses except the multivariable analysis. Children with late destructive PTLD had a trend towards better patient but not EF survival compared to those with early PTLD (p=0.16 & p=0.53, respectively) (Figure 1). Similarly, a trend was seen for worse 1-year patient but not EF survival in children with EBV+/early destructive PTLD compared to those with EBV+/late destructive & EBV-/late destructive PTLD (p=0.11 and p=0.46, respectively) (Figure 2). Children with EBV-/early destructive PTLD were excluded from this analysis due to small numbers. EBV tumor status, age at Tx, & organ transplanted and time from Tx to initial PTLD diagnosis were not identified as significant risk factors predicting 1-year mortality in multivariable analysis (p>0.10 for all variables).
Conclusion: Survival of non-destructive PTLD was high compared to those with destructive PTLD. A trend towards worse patient but not EF survival was seen for Destructive PTLD presenting early after Tx compared to those presenting later after Tx, although time to PTLD did not impact 1-year mortality in a multivariable analysis. EBV tumor status did not appear to impact mortality after late PTLD but there were not enough early EBV- tumors to assess its impact on outcome of early PTLD.
[1] PTLD
[2] EBV
[3] solid organ transplant
[4] Hematopoietic Stem Cell Transplant