Pediatric liver re-transplantation over 40 years: The largest comprehensive single-center experience
Fady M Kaldas1, Koki Maeda1, Minah Ha1, Robert S Venick1, Suzanne V McDiarmid1, Ryan Ma1, Samer S Ebaid1, Ronald W Busuttil1, Douglas G Farmer1.
1Department of Surgery, Division of Liver and Pancreas Transplantation, David Geffen School of Medicine at UCLA, Los Angeles, CA, United States
Objective: Liver retransplantation (ReLT) is the only curative option for children with liver allograft failure. Despite advances in surgical techniques and immunosuppression, ReLT remains challenging in children. Acuity-based allocation and organ scarcity have fueled skepticism of ReLT in many cases, limiting access to this life-saving intervention. In the present study, we aimed to 1) analyze a 40-year single-center experience with pediatric ReLT, 2) evaluate outcomes pre- and post-MELD/PELD, and 3) identify risk factors for early mortality.
Methods: All consecutive pediatric (≤18 y.o) ReLTs done at a single center were retrospectively analyzed. Comparisons were made pre-and post-implementation of MELD/PELD (1984 - 2001 vs. 2002 - 2023). Comparative and multivariable regression analyses assessed preoperative factors and identified predictors of early (death ≤ 12 months) mortality.
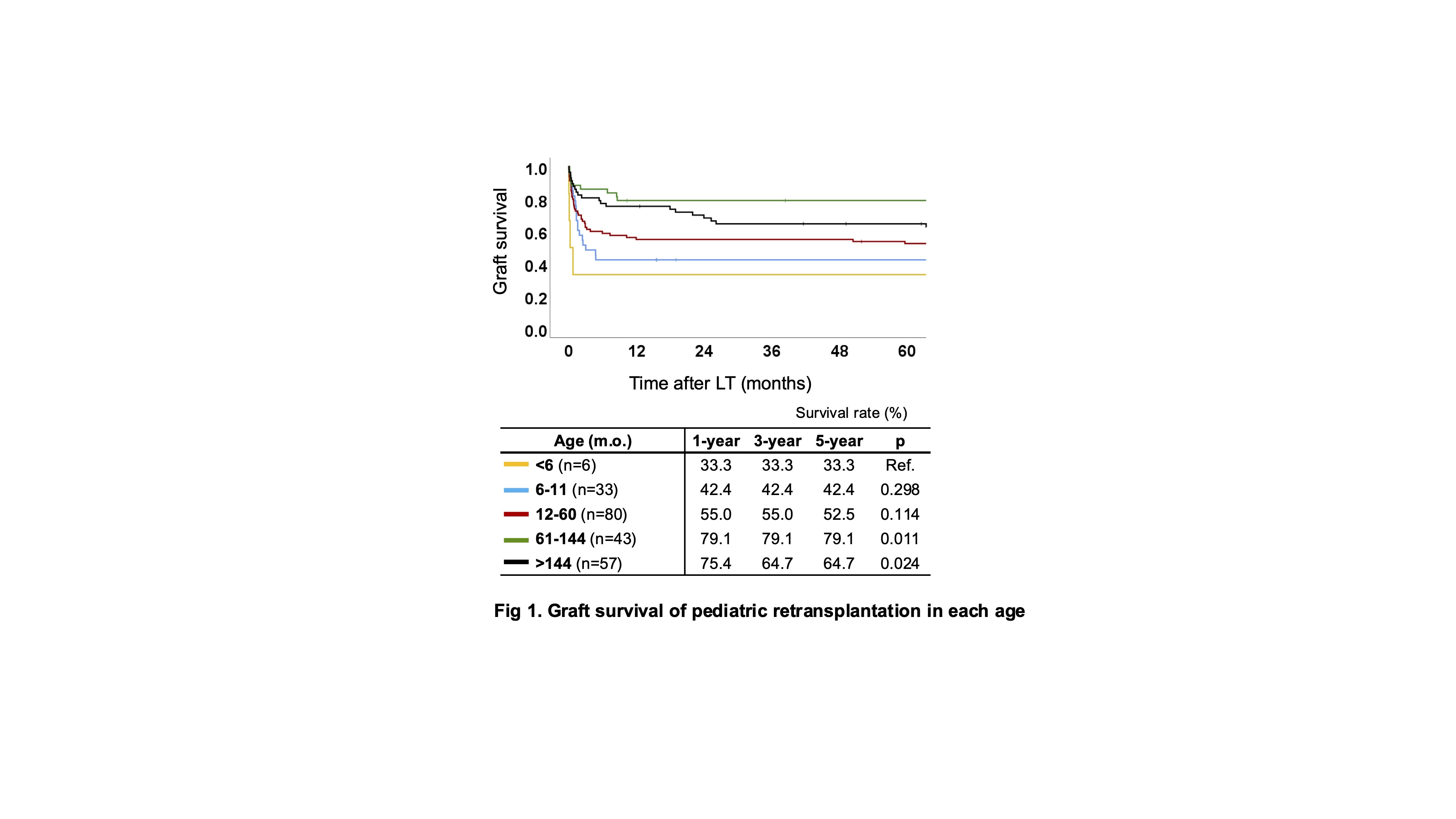
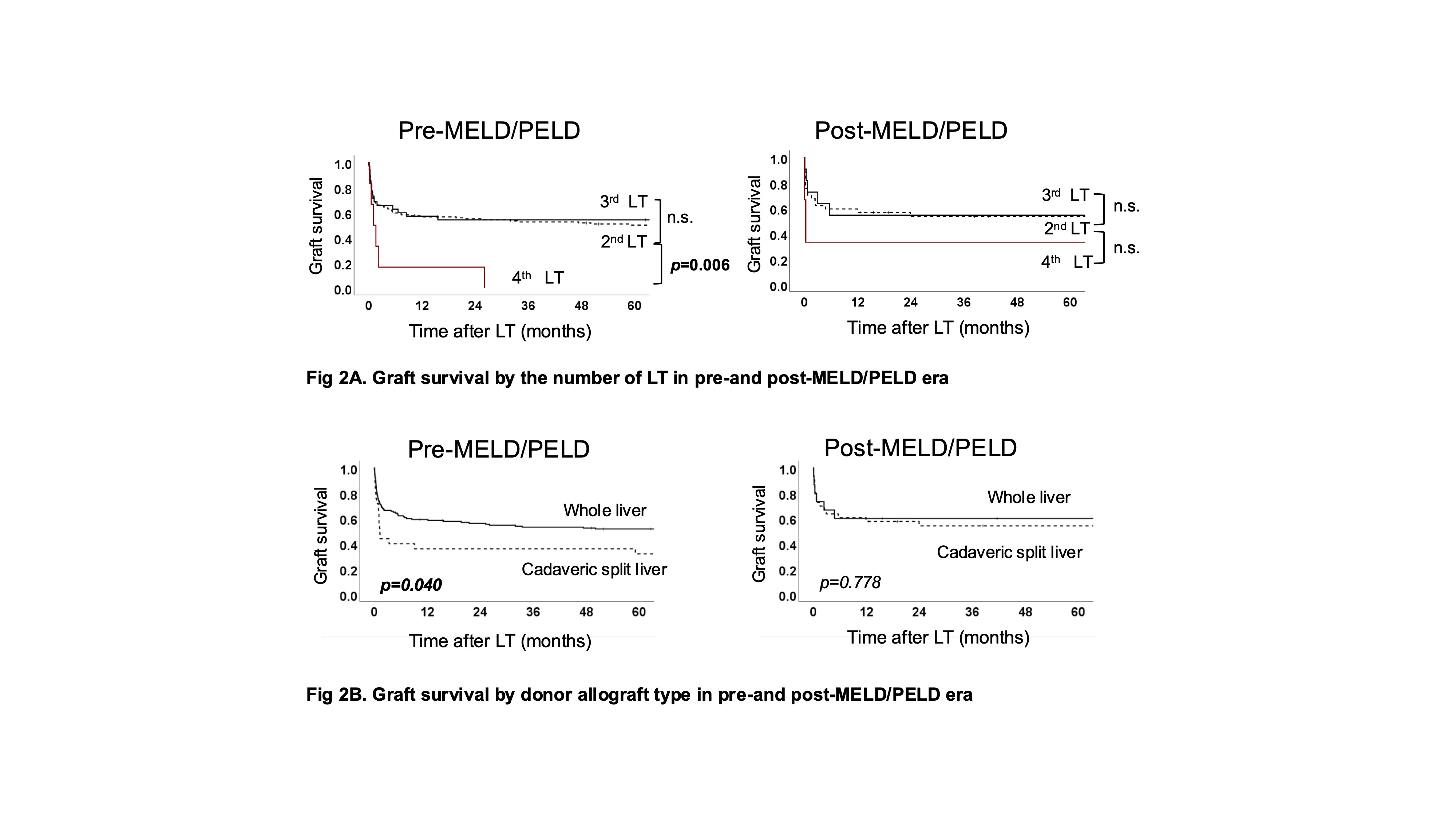
Results: 219 consecutive pediatric ReLTs were performed in 164 recipients over the study period (n=168 [76.7%] Pre-MELD/PELD and n=51 [23.3%] Post-MELD/PELD). The median age at ReLT was 4 y.o [1-12], and 46% of patients were male. The most common indications were vascular thrombosis (34.7%), rejection (28.3%), and primary non-function (PNF) (19.2%). 78% of patients had whole liver grafts, 18% had cadaveric split liver, and 4% had living donor liver grafts. Overall survival was 62.6%, 55.6%, and 51.2% at 5-, 10- and 20-years. Patient survival was best in ReLT for vascular thrombosis and rejection, and worst for PNF and delayed graft failure (> 7 days after prior LT). Graft survival at 1 year after a third LT (56.5%) was equivalent to the second LT (57.3%, p=0.710); however, it was better than the fourth LT (22.2%, p=0.004). Graft survival in the younger age groups was worse than in the older groups (Fig 1). Compared to pre-MELD/PELD ReLTs, more post-MELD/PELD ReLTs were for rejection. Post-MELD/PELD ReLT patients had more cadaveric split grafts (29.4 vs. 14.9%, p=0.019) and were more likely to require pre-op dialysis (25 vs. 12%, p=0.022). Although patients’ and graft survival in each era were equivalent, graft survival of the fourth LT and cadaveric split graft were significantly improved compared to their counterparts in the post-MELD/PELD era (Fig 2). Multivariate Cox regression of pre-operative variables identified recipient age <5 y.o ([HR; 95%CI] 2.189; 1.165-4.116, p=0.015), the fourth LT (9.292; 3.593-24.030, p<0.001), PNF (3.328; 1.763-6.281, p<0.001), and delayed graft failure (2.714; 1.148-6.416, p=0.023) as independent risk factors for early mortality.
Conclusion: To our knowledge, this represents the largest single-center pediatric ReLT experience. Despite the increased acuity and complexity of pediatric ReLT, outcomes of technically demanding ReLT have been improving. With careful patient selection and risk stratification, we can minimize futile outcomes and provide long-term survival of pediatric ReLT in an acuity-based allocation environment.