Retrospective analysis of Liver Transplantations in Biliary Atresia despite low bilirubin levels following Kasai procedure: Key insights
Carlotta Plessi1, Catherine de Magnée1, Aniss Channaoui1, Isabelle Scheers1, Giulia Jannone1, Xavier Stephenne1, Roberto Tambucci1.
1Pediatric Liver Transplantation Program, Cliniques Universitaires Saint-Luc - Université catholique de Louvain, Brussels, Belgium
Introduction: A normal serum bilirubin (SB) level is considered a primary and essential early outcome after the Kasai procedure (KP), and its association with higher native liver survival rates has been well-established. However, a significant number of children still require liver transplantation (LT), even after achieving stable clearance of hyperbilirubinemia following the procedure. The aim of this study is to assess the characteristics of patients with biliary atresia (BA) who underwent LT despite having persistent normal or subnormal total SB levels after KP.
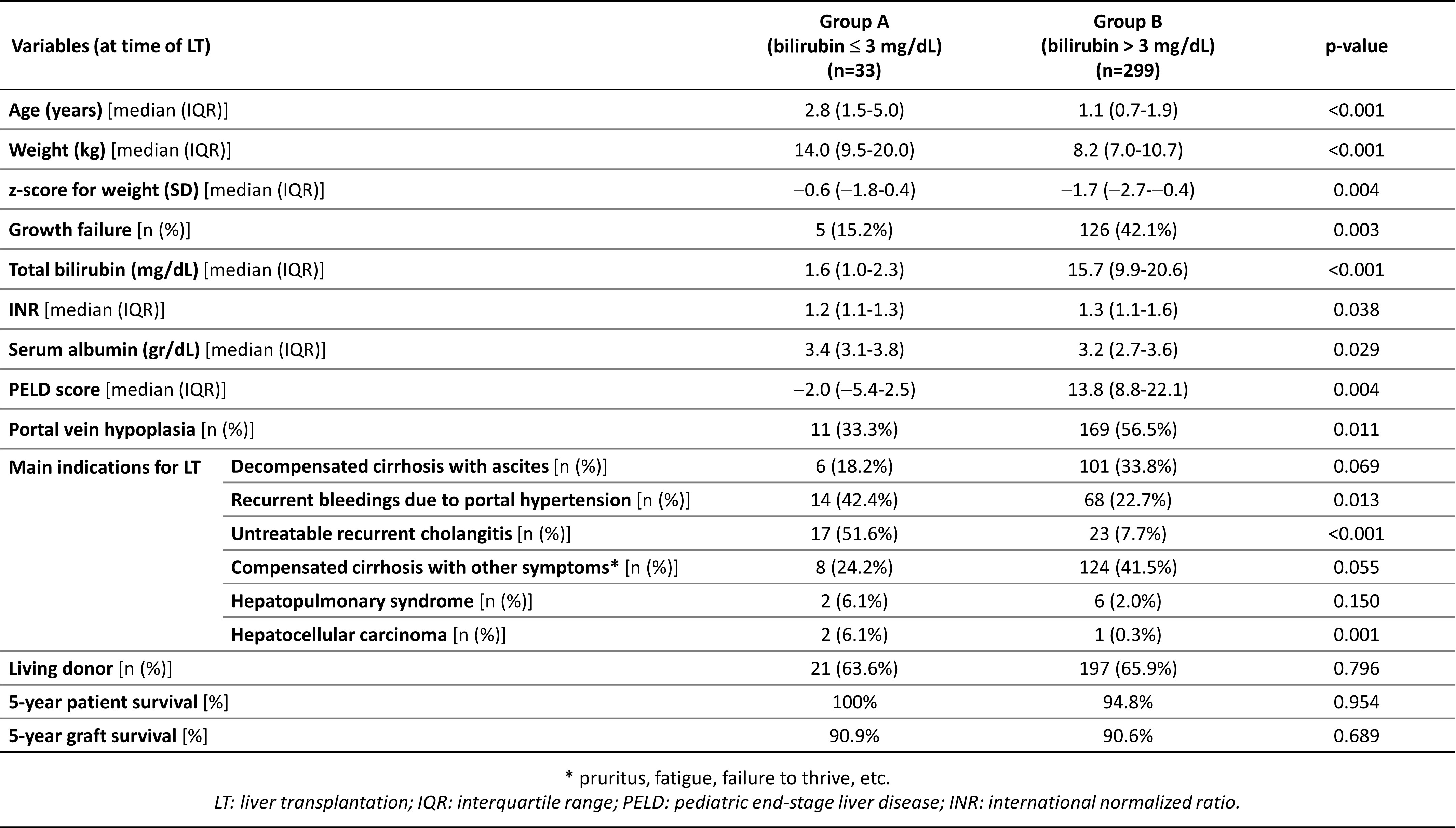
Methods: This is a single-center retrospective analysis of 443 pediatric recipients affected by BA who underwent LT between 1993 and 2022. Among them, those who had previously undergone KP were divided into two groups based on their SB levels at the time of LT: group A (SB ≤3 mg/dL) and group B (SB >3 mg/dL). The analysis included pre-LT characteristics, main indications for LT, and post-LT outcomes. The length of the pre-existing Roux-en-Y jejunal loop was assessed during LT, and it was considered inadequate if it was less than 30 cm.
Results: Of the 332 children (74.9%) who had received a previous KP, 33 (9.9%) had SB ≤3 mg/dL, including 10 with normal values (≤1.2 mg/dL). At the time of LT, patients in group A were significantly older, had a lower rate of growth failure, and had lower PELD scores (with differences observed in all PELD-computing variables). Regarding the main indications for LT, untreatable recurrent cholangitis, severe portal hypertension, and hepatocellular carcinoma were significantly more frequent in group A. The rate of ascitic decompensation was non-significantly higher in group B. During LT, 100 inadequate Roux-en-Y lengths were identified (median: 20 cm; IQR: 15-21 cm), which were more frequent in patients transplanted for recurrent cholangitis (61.1% vs 26.4%; p<0.001). There were no significant differences in patient and graft survivals between groups A and B.
Conclusion: A relevant number of BA patients underwent LT despite having normal or subnormal SB levels. Recurrent cholangitis was the primary indication for LT in these patients and was often associated with a short pre-existing Roux-en-Y. Interestingly, despite generally better clinical conditions, some patients with low SB levels underwent transplantation at a young age and/or due to decompensated cirrhosis with ascites.