Facing the issue of acute-on-chronic liver failure in pediatric biliary atresia: A prognostic and therapeutic challenge
Maria Julia Minetto1, Ivone Malla1,2, Stefania Conde1, Katherine Lancheros2, Esteban Halac1, Hayellen Reijenstein1, Agustina Jacobo Dillon1, Leandro Lauferman1, Diego Aredes1, Florencia Degrave1, Santiago Cervio1, Jose Calderon1, Mauro Capparelli3, Roxana Martinitto4, Natalia Pabon4, Daniel Buamscha5, Carlos Cambaceres5, Mauro García5, Susana López2, Oscar Imventarza1, Marcelo Dip1.
1Liver Transplantation, Garrahan Pediatric Hospital, Buenos Aires, Argentina; 2Hepatology, Garrahan Pediatric Hospital, Buenos Aires, Argentina; 3General surgery, Garrahan Pediatric Hospital, Buenos Aires, Argentina; 4Inpatient unit, Garrahan Pediatric Hospital, Buenos Aires, Argentina; 5Intensive care unit, Garrahan Pediatric Hospital, Buenos Aires, Argentina
Introduction: Acute-on-chronic liver failure (ACLF) is a severe complication of chronic liver disease that carries a high mortality rate. It manifests as an acute deterioration of liver function, triggered by infections or other insults, superimposed on the backdrop of chronic liver disease. Pediatric patients with biliary atresia (BA), a progressively cirrhotic cholangiopathy, are susceptible to ACLF and data in this group of age is scarce. The objective of this work is to report outcomes from patients with BA and ACLF treated at our center
Patients and methods: we retrospectively collected data of clinical charts from pediatric patients with BA presented in our center from February 2010 till December 2019 We analyzed clinical presentation, severity, management strategies and outcomes.
Results: of 200 patients with BA (31.5% males), 78 (39%) have suffered ACLF since 2010.
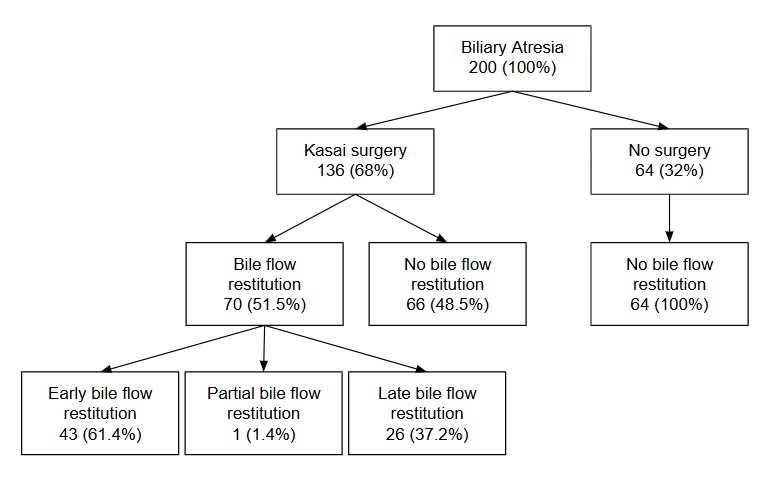
Median follow-up time was 6.52 years (range: 0.27-14.1 yr). 70/136 patients have recovered bile flow after Kasai surgery (KS) (51.5%). 89.7% of ACLF cases were stage 1, 85.9% had infections, 21.8% variceal bleeding. The median of PELD score at ACLF episode was 26 (range: 12-48). Lack of recovering bile flow (with or without KS) was a risk factor for ACLF (OR 16.6, 95% CI: 6.3-44.1 p 0.0001). 85.9% of patients with ACLF underwent liver transplant (LT) within the first month of ACLF episode, with 90% of 1yr survival. Eleven patients with ACLF episodes could not achieve LT (12%), 6 have died and 5 were lost from follow-up near the last episode. Patient survival at 1, 3 and 5 years was better for patients with BA without ACLF, compared to patients with ACLF (p value 0.01).
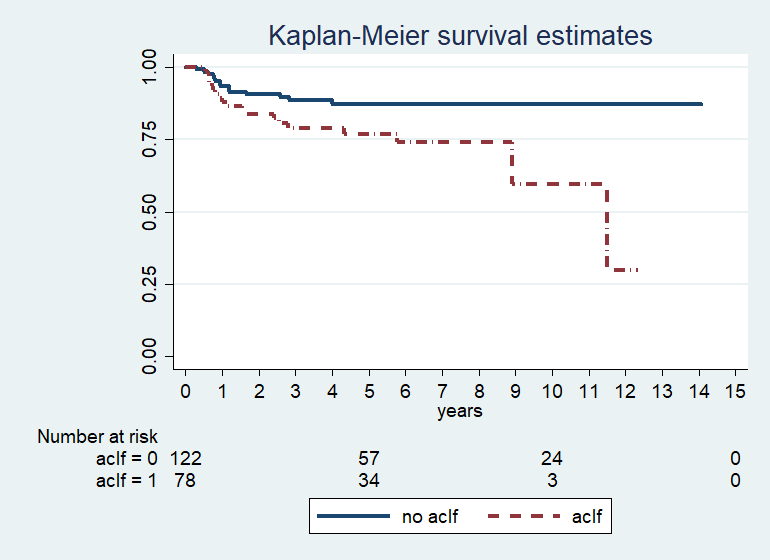
And among patients with ACLF, those who received a liver transplant had better survival than those who did not (p value 0.0001).
Conclusions: ACLF poses a significant clinical challenge in pediatric BA. In our series, with mild episodes, LT seems a therapeutic option that allows survival to this severe complication of children with chronic liver disease. Once lack of bile flow recovery is confirmed, shortening time to LT is of paramount importance to avoid the appearance of ACLF.
[1] acute-on-chronic liver failure
[2] biliary atresia