Proactive living donor liver transplant is associated with improved graft- and patient-survival outcomes in children with biliary atresia
Marshall Wallace1, Cameron Arkin1, Jean Botha2, Zachary Kastenberg1,2.
1Department of Surgery, Division of Pediatric Surgery, University of Utah Health, Salt Lake City, UT, United States; 2Pediatric Surgery, Intermountain Primary Children's Hospital, Salt Lake City, UT, United States
Introduction: Biliary atresia (BA) is the most common indication for pediatric liver transplantation (LT). Pediatric End-stage Liver Disease (PELD) scores primarily determine deceased donor transplant (DDT) waitlist priority. Due to persistent organ supply-demand mismatch, children typically have advanced disease, with high PELD scores, before DDT. A proactive approach to living donor liver transplant (LDLT) may facilitate early LT, before BA patients become critically ill, and may improve survival. We hypothesize that early LDLT, with a PELD of 12 or less, is associated with improved graft- and patient-survival in children with BA.
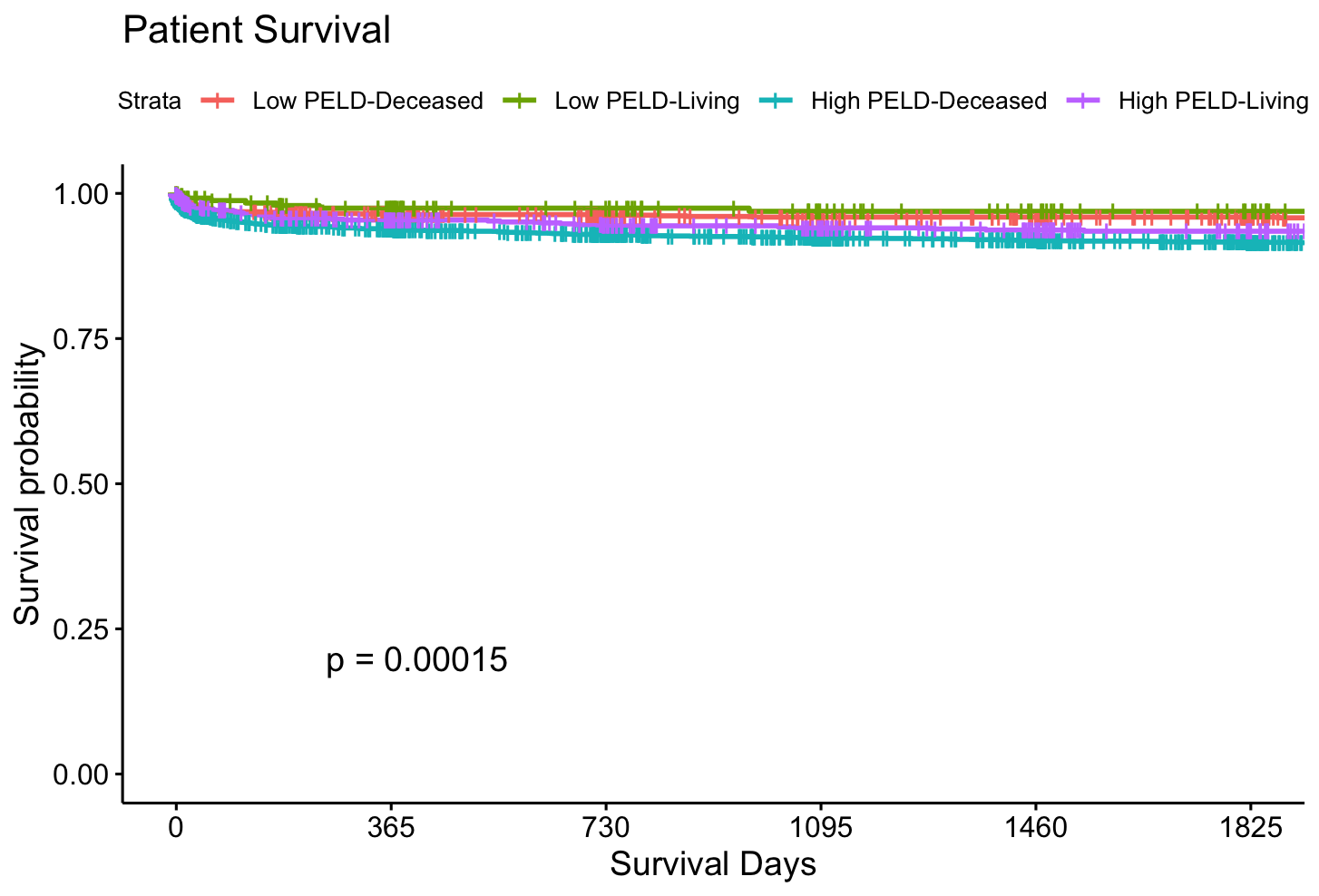
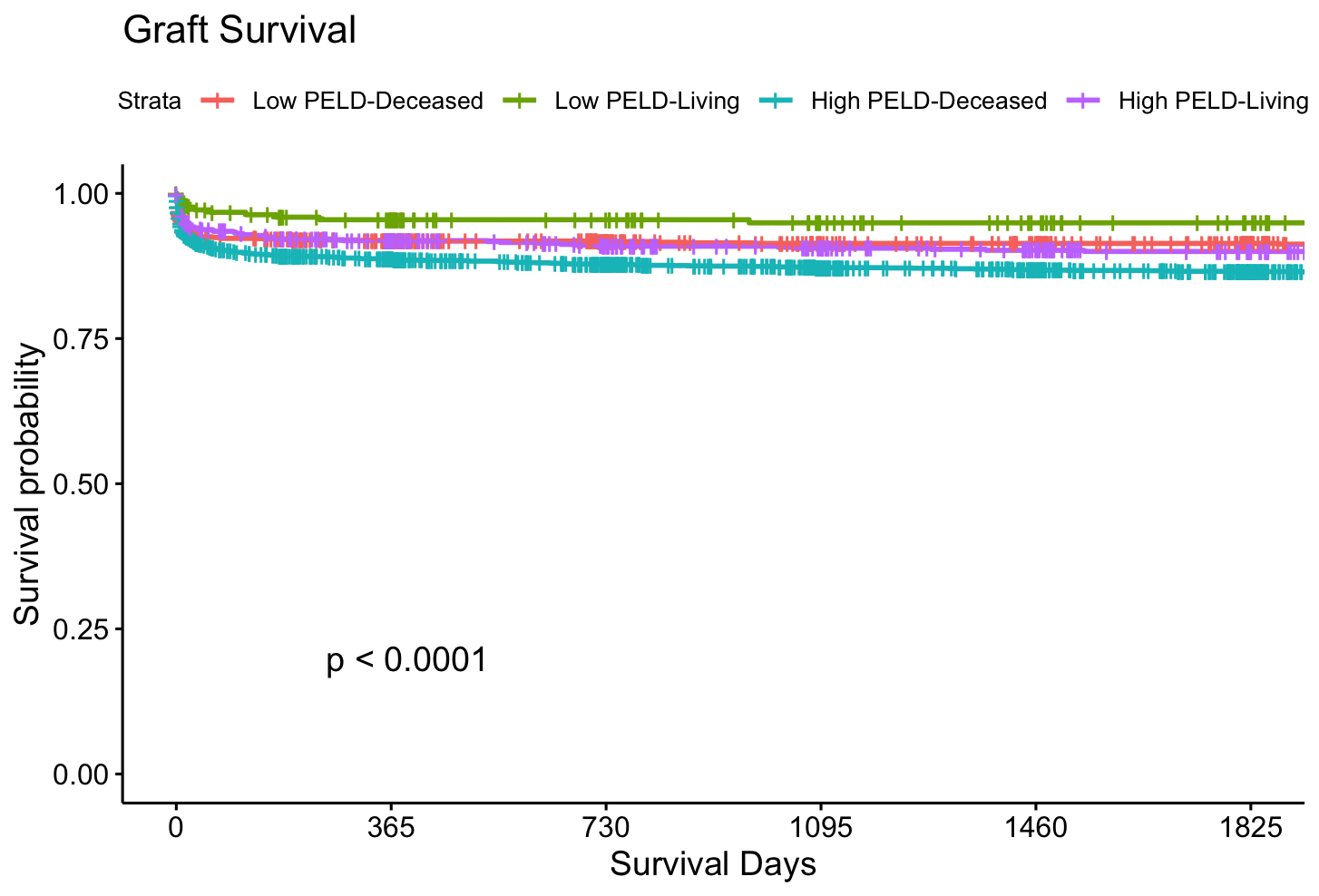
Methods: Retrospective review of children undergoing LT for BA in the United States Scientific Registry of Transplant Recipients (SRTR) database, comparing DDT and LDLT. Early, or low PELD, LT was defined as transplant with a PELD score of 12 or less. While high PELD LT was defined as transplant with a PELD of 13 or greater. Survival outcomes were tested using Kaplan-Meier analyses, while patient mortality and graft-loss were evaluated with Cox-proportional hazards analyses.
Results: 4,733 children were included (n=1152 – Low PELD-deceased donor, n=249 – Low PELD-living donor, n=2624 High PELD-deceased donor, n=708 High PELD-Living donor). Among the study cohort, the median age was 11 months, and the median weight was 8.2kg. Low PELD-living donor recipients had lower INR and bilirubin levels, and required less life support, prior to transplant (p<0.01). Using Kaplan-Meier analyses, long term graft- and patient-survival were significantly higher in the Low PELD-living donor cohort than in all other cohorts (p<0.01). Low PELD-living donor status was independently associated with decreased graft-loss (HR 0.43, p=<0.01) and patient-mortality (HR 0.42, p=0.02) with Cox proportional hazards modeling.
Conclusions: Living donor liver transplant is an effective strategy to increase the opportunity for liver transplantation and provides superior outcomes in children with biliary atresia. A proactive approach to LDLT should be considered in children with BA with low PELD scores.
[1] Biliary Atresia
[2] Living Donor Transplant