Impact of specific HLA-DR mismatches on de novo donor-specific antibody formation in pediatric kidney transplantation
Anika Shah1, Vaka Sigurjonsdottir2, Daniel Turudic 3, Paul Grimm1, Bing Zhang1.
1Stanford University , Stanford, CA, United States; 2University of Miami, Miami, FL, United States; 3University of Zagreb , Zagreb, Croatia
Introduction: While HLA-DRB1 mismatching has been widely studied in kidney transplantation, the relevance of HLA-DRB3, DRB4, and DRB5 remains underexplored. Advances in high-resolution HLA typing now allow more precise assessment of these mismatches, yet their potential impact on de novo donor-specific antibody (dnDSA) formation is unclear. This study aimed to evaluate the frequency of HLA-DRB1 vs. HLA-DRB3/4/5 mismatches and their association with dnDSA formation in pediatric kidney transplant recipients.
Methods: This retrospective cohort study included pediatric kidney transplant recipients from 2010–2018 at a single center, with follow-up through 2022. HLA typing was performed using high-resolution next-generation sequencing. Anti-HLA antibody testing was conducted pre-transplant, at 1, 2, 3, 6, and 12 months post-transplant, and when clinically indicated. dnDSA positivity was defined as MFI ≥3000, absent pre-transplant.
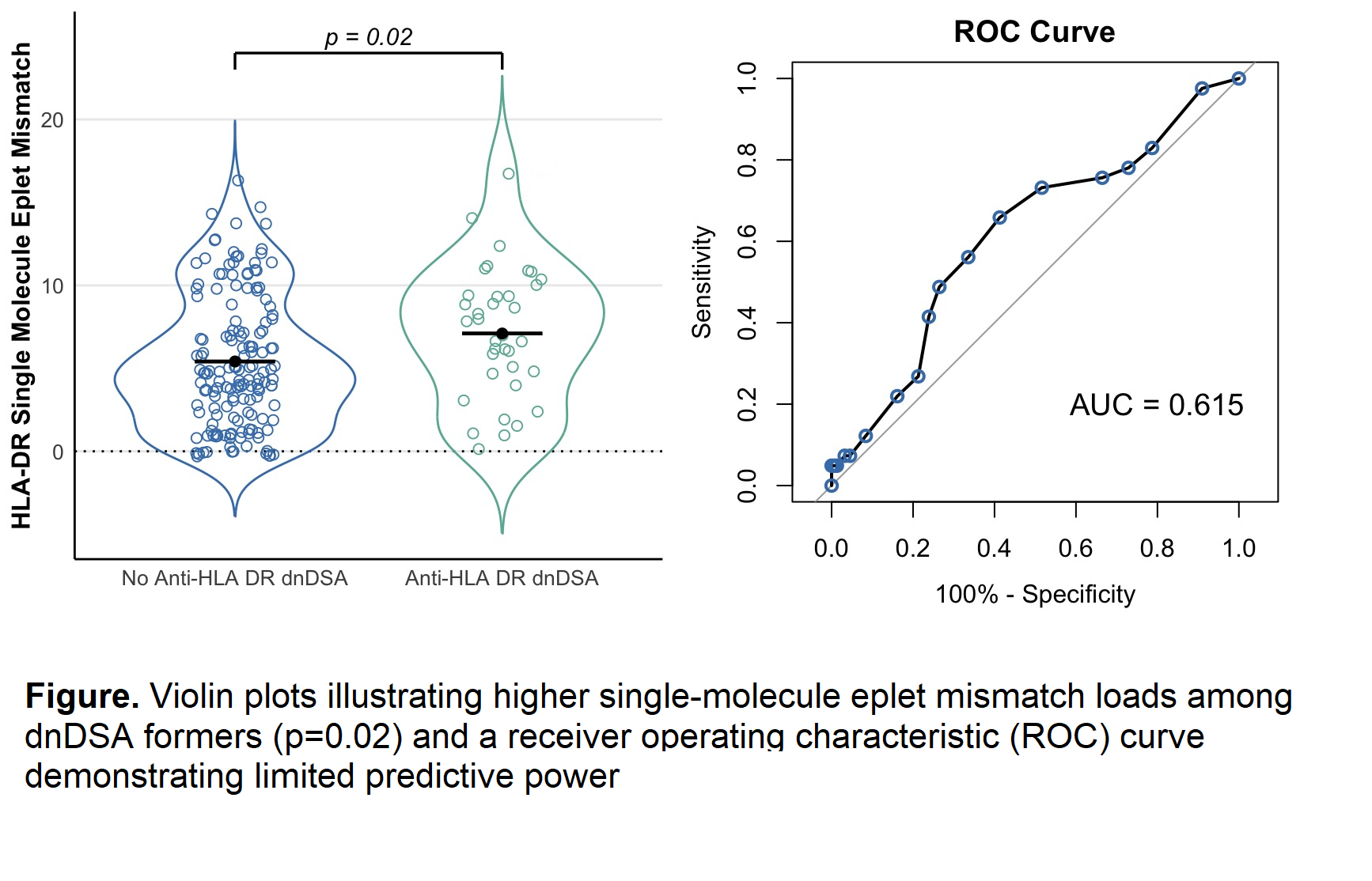
Eplet mismatches between donors and recipients were identified using HLA Matchmaker software (HLA DRDQDP Matching, 3.1.). Comparisons between groups were performed using Fisher’s exact test, Wilcoxon–Mann–Whitney test, and violin plots. Receiver operating characteristic (ROC) analysis was used to assess the predictive performance of eplet mismatch load for dnDSA formation.
Results: Among 227 pediatric kidney transplant recipients (median age: 14 years [IQR: 4–17], 49% female, 39% Hispanic/Latino), the median follow-up was 73 months [IQR: 58–96].
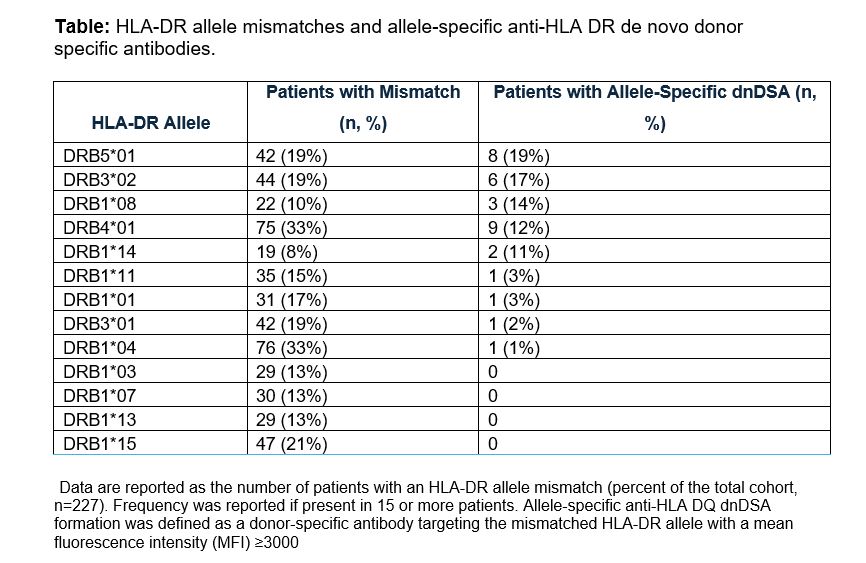
Seventy-three patients (32.2%) developed de novo Class II donor-specific antibodies (dnDSAs), including 65 (28.6%) with anti-HLA-DQ dnDSAs and 36 (15.8%) with anti-HLA-DR dnDSAs. HLA-DRB3/4/5 mismatches were associated with a higher rate of allele-specific dnDSA formation than HLA-DRB1 mismatches (11.7% vs. 2.6%, p < 0.001).
Violin plots show significantly higher single-molecule eplet mismatch loads among recipients who develop anti-HLA-DR dnDSA, but ROC analysis demonstrated limited predictive power for eplet mismatch load.
Conclusions: HLA-DRB3/4/5 mismatches were associated with higher rates of allele-specific dnDSA formation than HLA-DRB1 mismatches. Further investigation is needed to determine the clinical significance of DRB3/4/5 mismatches and whether incorporating DRB3/4/5 typing into transplant risk assessments could improve HLA matching strategies and enhance post-transplant risk stratification in pediatric kidney transplantation.