Carolina Magalhães Magalhães Costa, Brazil has been granted the IPTA Congress Scientific Awards

Double vs single hepatic artery anastomosis in pediatric left liver grafts: a reassessment of outcomes
Carolina Magalhães Costa1, Eduardo Antunes Fonseca 1, Renata Pereira Sustovich Pugliese 1, Marcel Ruiz Benavides1, Rodrigo Vincenzi 1, Karina Roda1, Nathália Rangel Porto Travassos1, Debora Puzzi Fernandes1, Teng Hsiang Wei1, Fernanda do Carmo Iwase 1, Mônica Lúcia Rodrigues 1, João Seda Neto 1.
1Hepatology and Liver Transplantation, Hospital Sírio-Libanês, São Paulo, Brazil
Background: The primary goal of hepatic artery (HA) reconstruction in liver transplants is to minimize the risk of hepatic artery thrombosis (HAT). Surgical approaches vary in the number of arterial anastomoses, magnification techniques, and anticoagulation strategies. This study analyzes the anatomical approaches used for arterial reconstruction, the incidence of HAT, and associated risk factors.
Method: A retrospective study of 489 primary pediatric LDLT performed between January 2017 and July 2024.
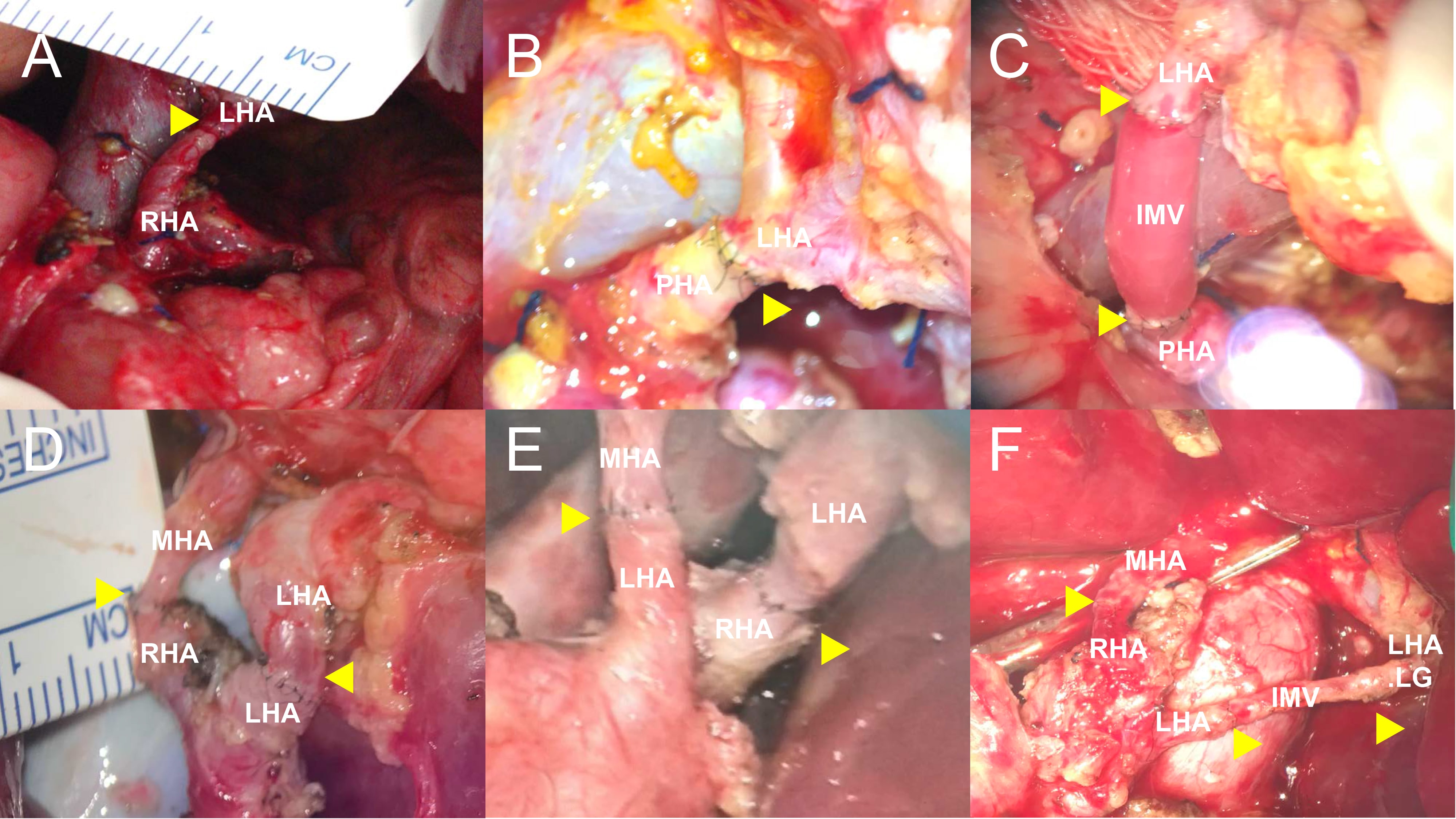
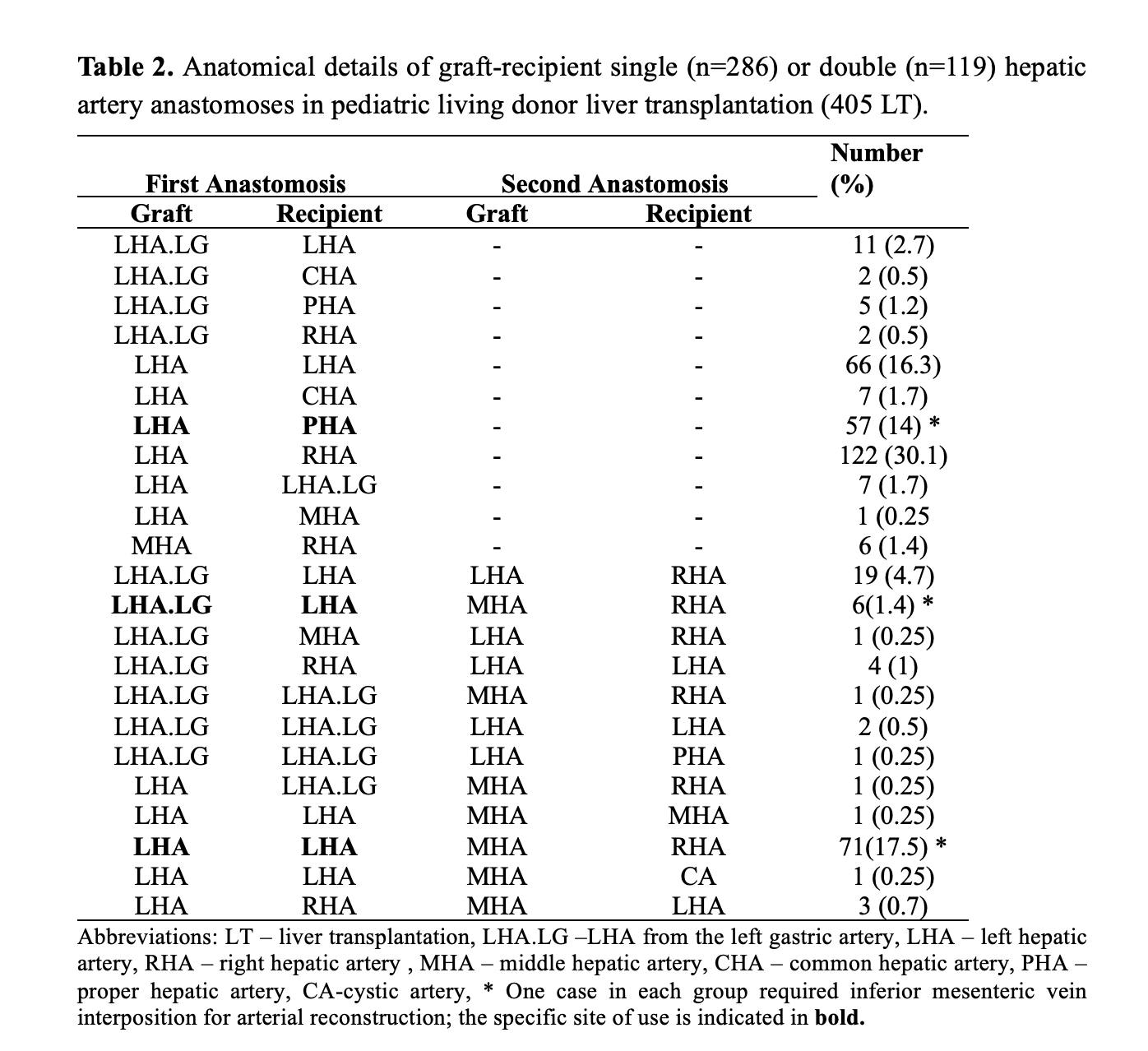
Results: The incidence rates of HAT, early portal vein thrombosis (EPVT), late-PVT, biliary leak (BL), and biliary stricture (BS) were 1% (n=5), 1.4% (n=7), 4.3% (n=21), 15% (n=73), and 11.9% (n=58), respectively. Double hepatic artery anastomosis was performed in 29.4% (119/405) of cases, with LHA-LHA + MHA-RHA being the most frequent combination (Figure 1 and 2). HAT occurred in four patients (1.4%) with single HA anastomosis and one patient (0.8%) in the double HA group (P=1.00). The rates of BS and BL in the single HA group were 14.7% (n=51) and 12.1% (n=42), respectively, compared to 16% (n=21) and 10.7% (n=14) in the double HA group (BS: P=0.72, BL: P=0.66). Increasing age and cold ischemia time were associated with higher HAT risk. The overall survival rate was 94.6%, with a median follow-up of 50.7 months (IQR: 21.1–73).
Conclusion: This study showed a low HAT rate (1%) with increasing age and cold ischemia time as risk factors. Double HA anastomosis did not reduce biliary complications. The most common arterial graft-recipient combinations in this study were LHA-RHA for single HA reconstruction and LHA-LHA + MHA-RHA for double HA reconstruction.
[1] Liver transplantation
[2] Hepatic artery thrombosis
[3] Children
[4] Outcomes
[5] Living donation
[6] Arterial reconstruction