Toward zero waitlist mortality: A mixed-methods review of loss of life while awaiting pediatric liver transplant
Joshua Gossett1, Noel Thompson2, Mihaela Damian3, Regino Gonzalez-Peralta4, John Bucuvalas5, Carrie Smith6, George Mazariegos2.
1Pediatric Transplant Center, Stanford Medicine Children's Health, Palo Alto, CA, United States; 2Transplant Services, UPMC Children’s Hospital of Pittsburgh, Pittsburgh, PA, United States; 3Pediatric Intensive Care Unit, Arthur M Blank Hospital, Children's Healthcare Atlanta, Atlanta, GA, United States; 4Pediatric Gastroenterology, AdventHealth Medical Group, Orlando, FL, United States; 5Pediatric Hepatology, Mount Sinai Kravis Children’s Hospital, New York, NY, United States; 6Transplant Services, Texas Children's Hospital, Houston, TX, United States
Purpose: The Starzl Network aims to give all children access to the best care and has committed to achieving zero waitlist mortality in those awaiting liver transplant. We looked to apply improvement science processes to a sample of recent waitlist mortality cases with the intent to extract meaningful and actionable themes that can drive forward projects aimed at eliminating deaths of those awaiting pediatric liver transplantation.
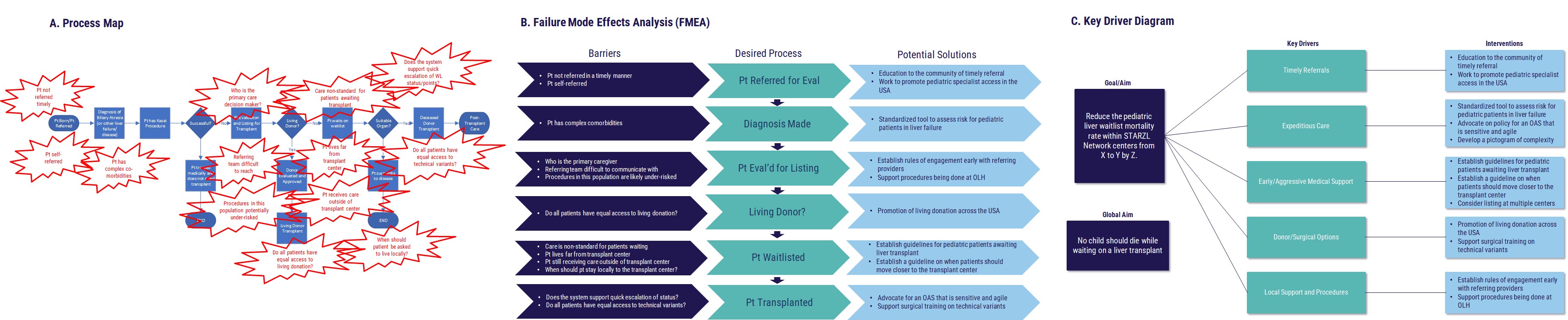
Methods: A base qualitative interviewing structure was created and continuous improvement was applied that altered and enriched the process including 1) introduction of additional interview settings and 2) inclusion of new participants such as patient family representatives. Templated questions were developed and modified as themes began to emerge from the reviews. Interviews were multi-phased and increased in number of participants as they progressed to provide safety and support. Each case went through 3-4 separate interviews with varying participants to extract the maximum amount of discussion and theme identification. Recurring concepts were identified, databased, and applied in aggregate to quality improvement (QI) tools, including failure modes and effects analysis (FMEA), process maps, and key driver diagrams.
Results: Six cases have been reviewed from across the US and Canada. Age range of the case subjects ranged from 3 weeks to 14 years. An average of 5 themes were identified in each case (range of 4-8) with major discussion points in each review. Between 0-4 QI recommendations were provided for the process in each review and were iteratively applied to future cases and interviews. A process map, FMEA and key driver diagram were created and contributed to as case reviews progressed. (see Figure)
Conclusions: Utilizing mixed method interview structures, we identified commonalities among pediatric waitlist mortality cases. Furthermore, we propose future opportunities to act at a center level, and national policy level, toward eliminating the death of children awaiting transplantation.
References:
[1] Pediatrics
[2] Liver Transplant
[3] Waitlist Mortality
Lectures by Joshua E Gossett
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Thu-18 17:00 - 18:00 |
Immunosuppression, Ethical, Quality Improvement and Allied Health Posters - from P1.55 to P1.71 | Toward zero waitlist mortality: A mixed-methods review of loss of life while awaiting pediatric liver transplant | MOA 10 (Exhibit Area) |
