Use of parenteral nutrition prior to heart transplantation for Protein-losing enteropathy related to Fontan circulation: Patient and clinician perspectives at critical timepoints
Amy Andrews1, Kim Herbison1, Bryan Mitchelson2, John Stirling2, Helen M Evans1, Jonathan Bishop1.
1Paediatric Gastroenterology and Hepatology Service, Starship Child Health, Auckland, New Zealand; 2Paediatric and Congenital Cardiac Service, Starship Child Health, Auckland, New Zealand
Introduction: Protein-losing enteropathy (PLE) is a rare complication following Fontan surgery and is an indication for heart transplantation when symptoms are refractory to maximal medical therapy. Severe symptoms can result in malnutrition and micronutrient deficiencies that cannot be corrected without parenteral nutrition (PN).
Methods: A retrospective medical record review identified critical timepoints before and after heart transplantation in a teenager with Fontan circulation related PLE. The impact of nutritional status and management was considered from different perspectives, including the experiences of the patient, their caregivers and multi-disciplinary healthcare teams.
Results: A 17-year-old male with severe PLE first presented with PLE at age eight, two years after Fontan completion for pulmonary atresia with intact ventricular septum and a severely hypoplastic right ventricle. Symptoms of PLE were stable for many years with octreotide use, but he developed severe hypoalbuminemia (Albumin 12 g/L , Fecal Alpha-1-antitrypsin 7.2 mg/g), constitutional growth delay, thrombophilia and immune compromise with low IgG and IgA levels.
The patient was listed for heart transplantation with significant concern from the multi-disciplinary healthcare teams regarding his sub-optimal nutritional status and exercise tolerance. Despite optimization of nutrition support strategies, PLE severity prevented effective treatment of malnutrition with enteral nutrition. Further deterioration in nutritional status resulted in suspension from the heart transplantation waitlist and necessitated the need for PN. Use of PN with transition to home PN given overnight and daily for three months improved protein loss, nutritional status, exercise tolerance, quality of life and achieved relisting for transplantation. Heart transplantation occurred five months after initial listing. PN was required in the post-operative period until PLE and malnutrition fully resolved three months after transplantation.
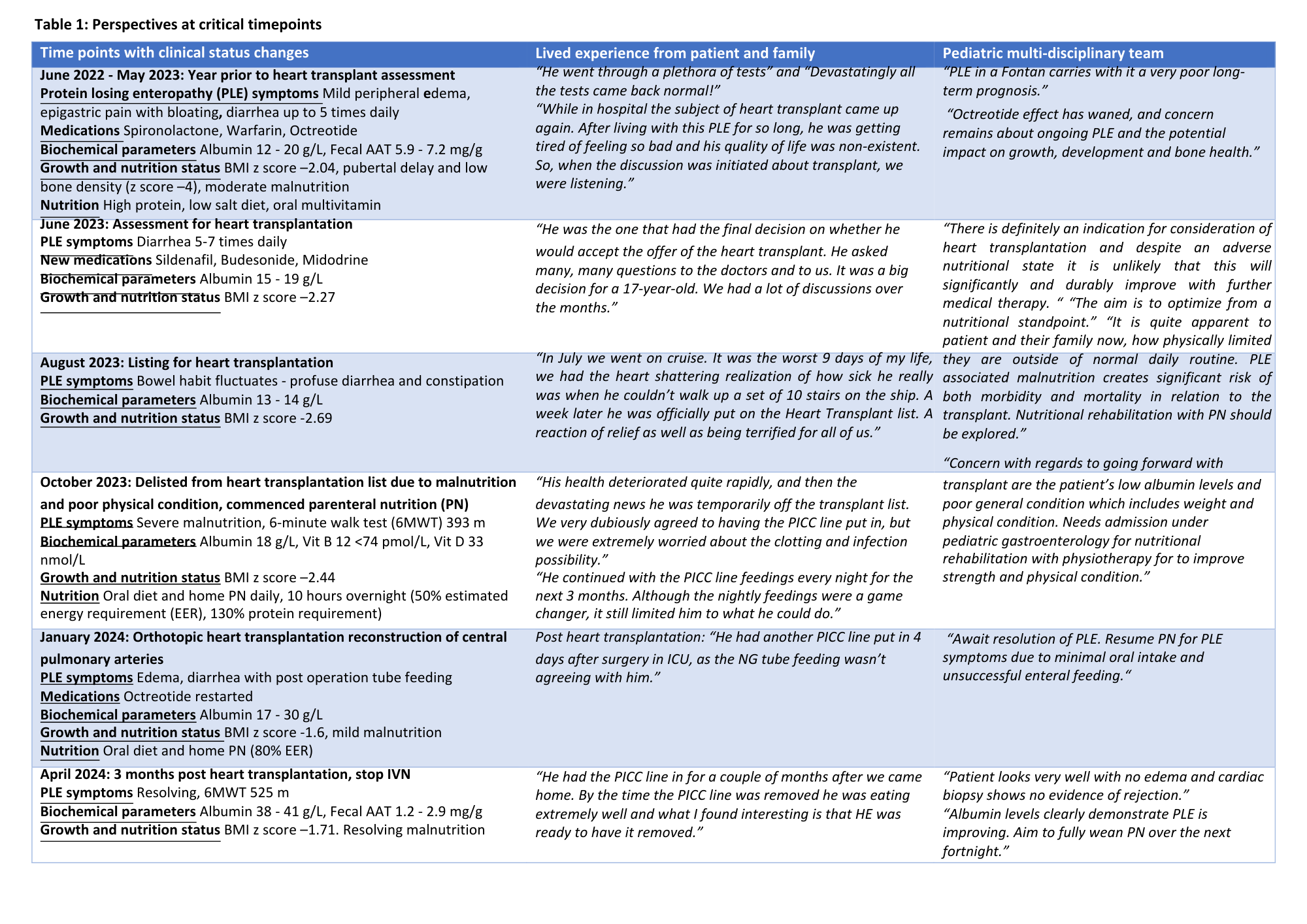
Given the burden of care of severe PLE requiring PN, partnering to plan and provide treatment for a young adult at transition age and his caregivers was essential. Consideration of their perspectives at critical timepoints (refer to Table 1) contributed to a more balanced treating team and patient relationship with achievement of relisting for heart transplantation and eventual positive health outcome.
Conclusion: This case demonstrates effective use of PN in a complex case of Fontan circulation related PLE and the importance of listening to the patient voice. Multi-disciplinary healthcare teams offered their perspectives in collaboration with a patient transitioning to adulthood. This provided a robust process of clinical decision-making regarding nutrition support to achieve a positive outcome.
References:
[1] Protein-losing enteropathy
[2] Fontan circulation
[3] Parenteral nutrition
[4] Patient experience
[5] Transition to adult care
[6] Heart transplantation
[7] Malnutrition
[8] Case report
Lectures by Amy Andrews
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Thu-18 17:00 - 18:00 |
Immunosuppression, Ethical, Quality Improvement and Allied Health Posters - from P1.55 to P1.71 | Use of parenteral nutrition prior to heart transplantation for Protein-losing enteropathy related to Fontan circulation: patient and clinician perspectives at critical timepoints | MOA 10 (Exhibit Area) |
