Vascular complications in children receiving a size-match whole liver transplant
Irene Dieguez1, Areej Muhammad1, Alba Bueno1, Hector Vilca-Melendez1,2, Rebeca Mateos1,2, Girish Gupte1, Khalid Sharif1.
1Liver Unit, Birmingham Children´s Hospital, Birmingham, United Kingdom; 2Liver Unit, Queen Elizabeth Hospital, Birmingham, United Kingdom
Introduction: Liver transplant is gold standard for end-stage chronic liver disease and some acute liver failures. Whole liver transplant (WLT) offers some advantages (logistically, technically and possibly functionally) compared to reduced/split/living donor. Evidence regarding complications in children WLT is still inconclusive.
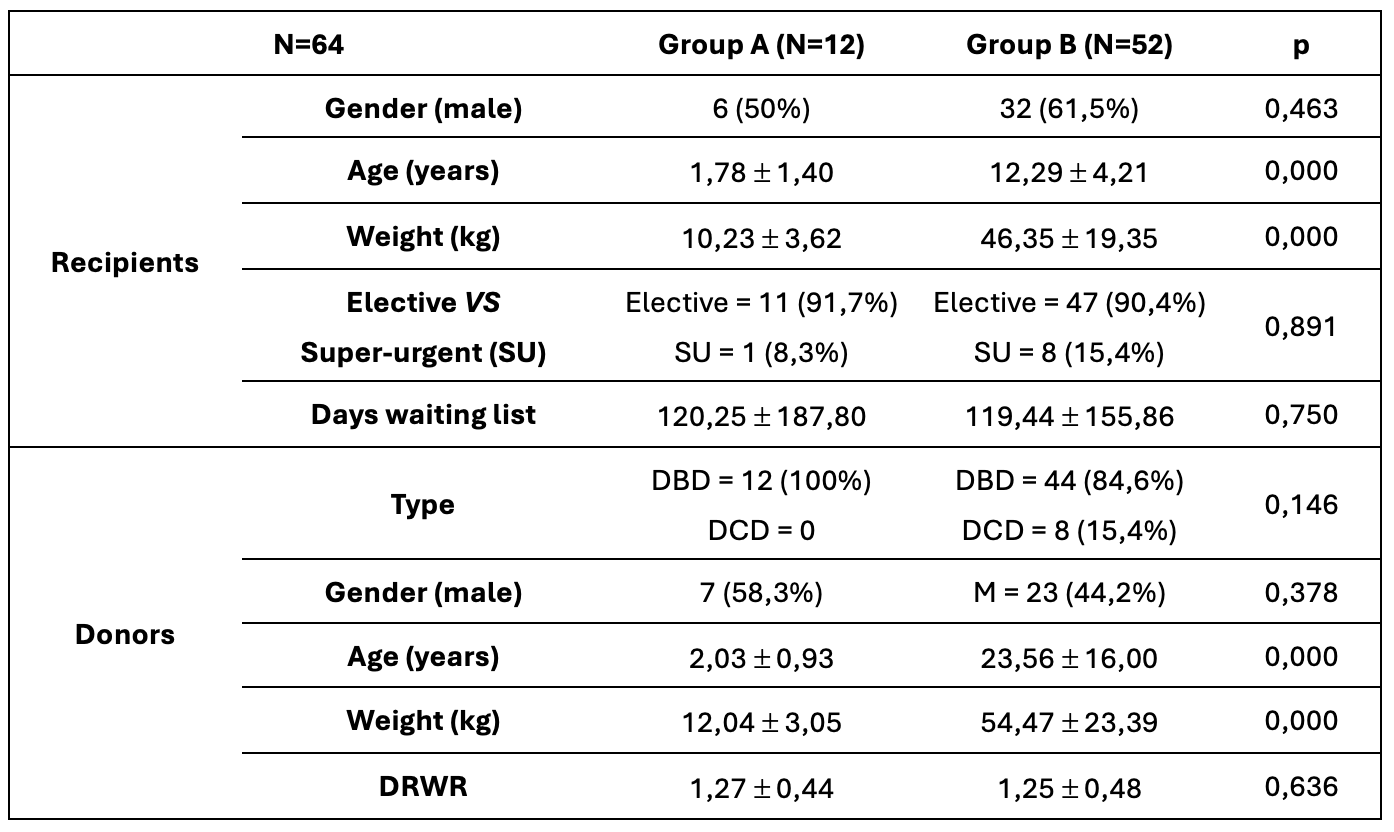
Methods: retrospective, cross-sectional study on patients <19 years old who received a WLT between 2000-2024. Exclusion criteria: redo. N=64, classified according to the donor’s weight in: A (≤15 kg) and B (>15 kg).
Studied variables: recipient and donor gender, age and weight, donor-recipient-weight-ratio (DRWR), indication, elective/super-urgent, ischemia times, surgical technique, early hepatic artery thrombosis (HAT), portal vein thrombosis (PVT) and need for super-urgent re-transplantation (30 days post-surgery).
Qualitative variables were described as absolute frequency and percentage cross-sectional test was used. Quantitative variables were described as mean and standard deviation and U-Mann-Whitney test was used. Statistical significance: p<0.05.
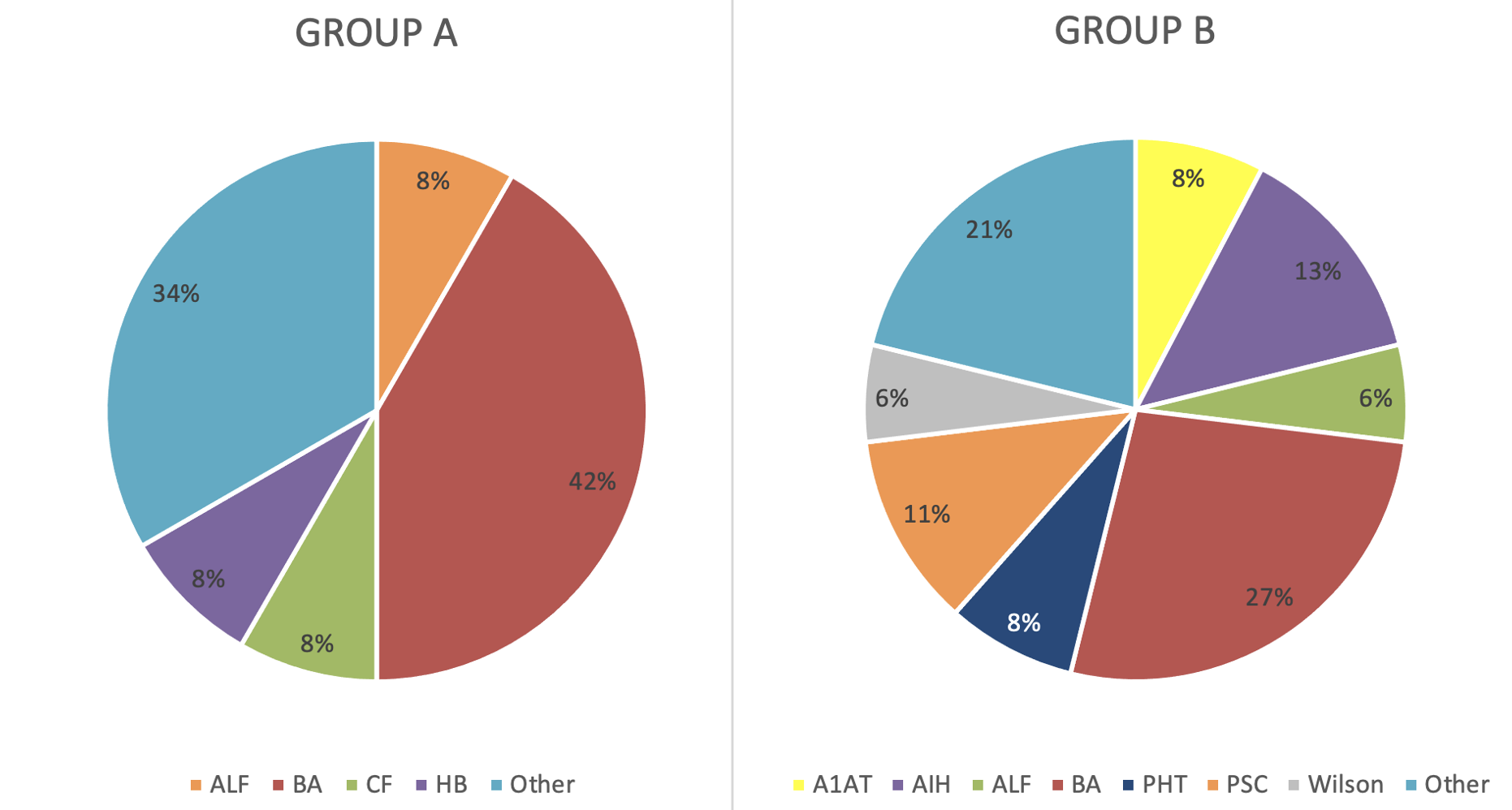
Results: group A (N=12, 18.75%) had lower age (1.78 ± 1.40 vs 12.29 ± 4.21; p<0.05) and weight (10.23 ± 3.62 vs 46.35 ± 19.35; p<0.05), as did their donors [(age: 2.03 ± 0.93 vs 23.56 ± 16.00; p<0.05. Weight (12.04 ± 3.05 vs 54.47 ±23.39; p<0.05). However, both groups were comparable in terms of gender, elective/super-urgent, DRWR, cold and warm ischemia times and surgical technique (piggy-back/classical technique, end-end /graft in portal vein and hepatic artery, and roux-loop/end-end biliary anastomosis). Biliary atresia was the most frequent indication in group A (41.7%), while group B was more diverse.
Regarding complications, there was higher incidence of HAT (N=3, 25% vs N=3, 6.12%; p=0.039), PVT (N=2, 16.67% vs N=1, 1.92%; p=0.0029)) and re-transplantation (N=2, 16.67% vs N=0, 0%; p=0.03) in patients receiving WLT from donors ≤15 kg.
Conclusion: children transplanted with a WLT have a higher risk of developing early vascular complications and necessity for super-urgent re-transplantation. Therefore, the acceptance of thse grafts should be carefully considered at the time of the offer.
References:
[1] Liver transplantation
[2] Full graft
[3] Hepatic artery thrombosis
[4] Portal vein thrombosis
[5] Retransplantation
Lectures by Irene Dieguez
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Thu-18 17:00 - 18:00 |
Liver/Intestine Posters - from P1.35 to P1.53 | Vascular complications in children receiving a size-match whole liver transplant | MOA 10 (Exhibit Area) |
