Henny A Puspitasari, Indonesia
Pediatric Nephrologist
Division of Nephrology, Department of Child Health
Faculty of Medicine Universitas Indonesia, dr. Cipto Mangunkusumo General Hospital
Cardiovascular profile of children with end-stage kidney disease prior to living donor kidney transplantation
Henny Puspitasari1, Sarah R Nursyirwan1, Intan D Puspitasari1, Eka L Hidayati1, Jeannine von der Born2, Anette Melk2.
1Department of Child Health, Faculty of Medicine Universitas Indonesia, dr. Cipto Mangunkusumo General Hospital, Jakarta, Indonesia; 2Department of Pediatric Kidney, Liver and Metabolic Diseases, Hannover Medical School, Hannover, Germany
Introduction: The most common cause of death in children after pediatric kidney transplantation (KTx) are cardiovascular (CV) complications. This study aims to describe the CV risk profile in ESKD children in Indonesia before KTx and analyze how it affects patient survival after transplantation.
Methods: This was a retrospective observational study held by the Division of Nephrology, Department of Child Health at dr. Cipto Mangunkusumo General Hospital, Indonesia. Participants were pediatric recipients of living donor KTx from January 2023-2025. Data recorded from medical records included demographic data, office blood pressure, hemoglobin level (Hb) and echocardiographic parameters: left ventricular (LV) ejection fraction (LVEF), LV mass index for height (LVMI, according to Chinali et al.), fractional shortening (FS), tricuspid annular plane systolic excursion (TAPSE), and E/A-ratio of mitral valve inflow. The data from the last documented echocardiography before KTx were used, mean 63 days (range 1-424 days) before KTx.
Results: A total of 41 children were included, 28 (68.3%) male, mean age was 14.4±3 years. Most patients were anemic with a mean Hb of 10 ± 2.4 g/dl. Median percentile of systolic blood pressure (SBP) and diastolic blood pressure (DBP) were 98th (range: 39th – 99th) and 96th (range: 61st – 99th), 73.2% (n = 30/41) displayed arterial Hypertension, in which 53.7% and 19.5% of patients were categorized into stage 2 and stage 1 hypertension respectively, 22 (54%) displayed left ventricular hypertrophy. After KTx 11/41 (27%) patients deceased caused by infection (6/11, 54.5%), CV complications (2/11, 18.2%) and others (3/11, 27.3%). Table 1 gives a first impression of important differences between surviving and deceased patients: deceased patients showed a higher mean SBP and DBP and a higher LVMI, all patients who died had left ventricular hypertrophy pre-KTx.
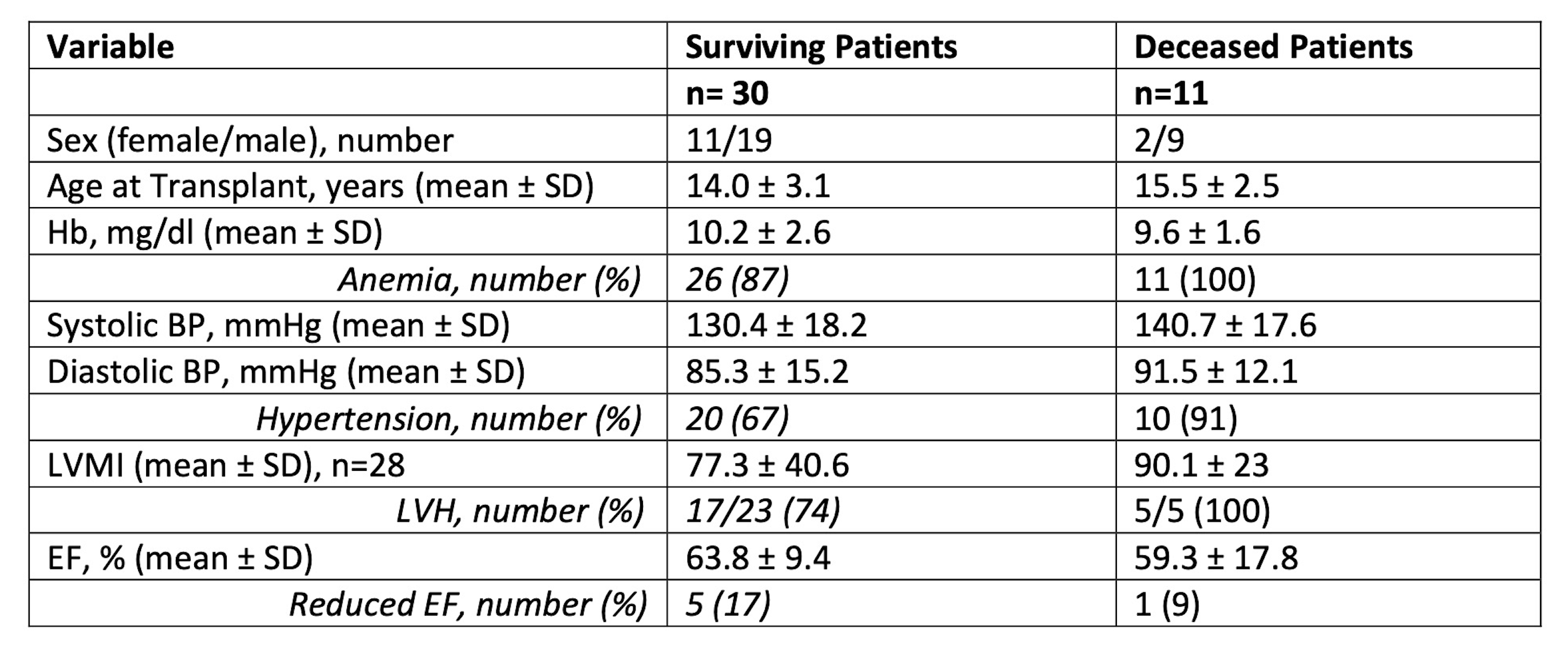
Conclusion: Children who died after KTx already appear to have a worse CV risk profile before KTx. We are actually planning to analyze associations of the pre-KTx CV risk profile with the survival after KTx. Multivariable analyses might reveal further associations with additional CV parameters. Given the severity of illness in the deceased patients, one possible outcome may be that children need to be transplanted at an earlier stage.
We would like to express our gratitude to Prof. Sudung O. Pardede, MD, Reza Fahlevi, MD, and the pediatric dialysis nurses at Dr. Cipto Mangunkusumo General Hospital for their help in coordinating, monitoring and maintaining data of kidney transplantation children. We would also thank Safitri Maulidina, MD, for her support in our data recruitment and analysis..
References:
[1] Cardiovascular risk
[2] children
[3] kidney
[4] transplantation
[5] survival
Lectures by Henny A Puspitasari
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Thu-18 17:00 - 18:00 |
Kidney Posters - from P1.1 to P1.32 | Cardiovascular profile of children with end-stage kidney disease prior to living donor kidney transplantation | MOA 10 (Exhibit Area) |
|
Sat-20 11:05 - 12:05 |
Tips for early career professionals | Short presentations from the 1st cycle of IPTA mentoring | MOA 6 |