Jianming Li, People's Republic of China
The First Affiliated Hospital of Sun Yat-sen University
Clinical outcomes of switching from tacrolimus to cyclosporine a in pediatric kidney transplant recipients with BK virus infection
Jianming Li1, Zicong Li1, Yusen Lin1, Huanxi Zhang1, Chenglin Wu1, Jun Li1, Qian Fu1, Gang Huang1, Longshan Liu1, Changxi Wang1.
1Organ Transplant Center, The First Affiliated Hospital of Sun Yat-sen University, Guangzhou, People's Republic of China
Background: BK polyomavirus-associated nephropathy (BKPyVAN) remains a major contributor to graft loss in pediatric kidney transplant recipients. This study aimed to identify clinical risk factors associated with BK virus (BKV) infection and to evaluate the efficacy and safety of switching immunosuppression from tacrolimus to cyclosporine A ((Tac-to-CsA)) in patients with high-level BK viruria (>10⁷copies/mL).
Methods: We performed a retrospective analysis of data from 472 pediatric kidney transplant recipients treated at the First Affiliated Hospital of Sun Yat-sen University, with a median follow-up duration of 4.42 years (range: 1–10 years). Among 55 recipients presenting with high-level BK viruria, we compared BKV clearance outcomes between those receiving conventional immunosuppressive therapy and those who underwent switching from tacrolimus to cyclosporine A.
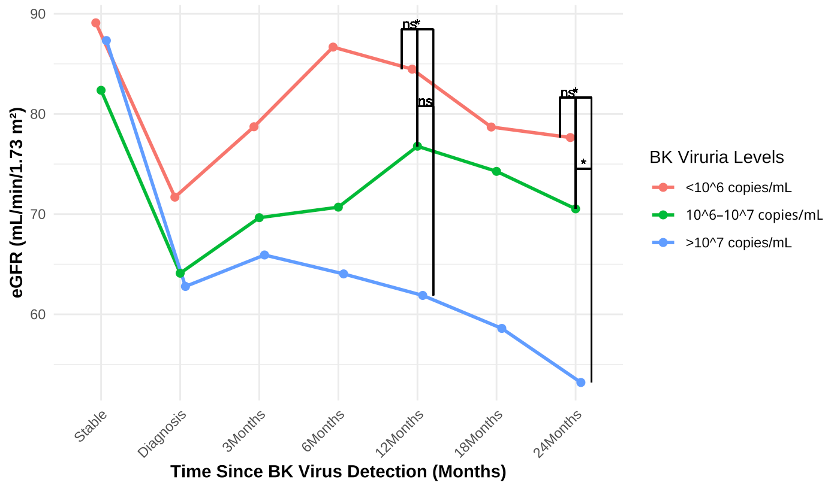
Results: BKV infection occurred in 86 recipients (18.2%), including 55 (11.7%) with high-level viruria, 8 (1.7%) with viremia, and 10 (2.1%) with biopsy-confirmed BKPyVAN. Notably, five of the BKPyVAN recipients had negative plasma BKV-DNA results. According to multivariable logistic regression analysis, recipient age <5 years (OR = 6.05, p < 0.01), donor age ≥5 years (OR = 4.50, p < 0.01), and obstructive uropathy as the primary renal disease (OR = 4.95, p = 0.02) were independently associated with an increased risk of high-level viruria. In addition, treatment for acute rejection (OR = 4.45, p = 0.03) and obstructive uropathy (OR = 14.01, p < 0.01) were significant predictors of BKPyVAN. Recipients with high-level viruria exhibited significantly lower estimated glomerular filtration rates (eGFR) at 12 and 24 months post-transplant compared to those without high-level viruria.
Among the high-level viruria group, progression to BKPyVAN was significantly associated with BK viremia (OR = 7.40, p = 0.05) and history of acute rejection treatment (OR = 6.80, p = 0.06). Importantly, switching from tacrolimus to cyclosporine A significantly reduced the risk of BKPyVAN (OR = 0.07, p = 0.03). Recipients who underwent switching from tacrolimus to cyclosporine A demonstrated significantly improved BKV clearance and a markedly lower incidence of BKPyVAN relative to those maintained on standard immunosuppression (3.7% vs. 28.6%, p = 0.02).
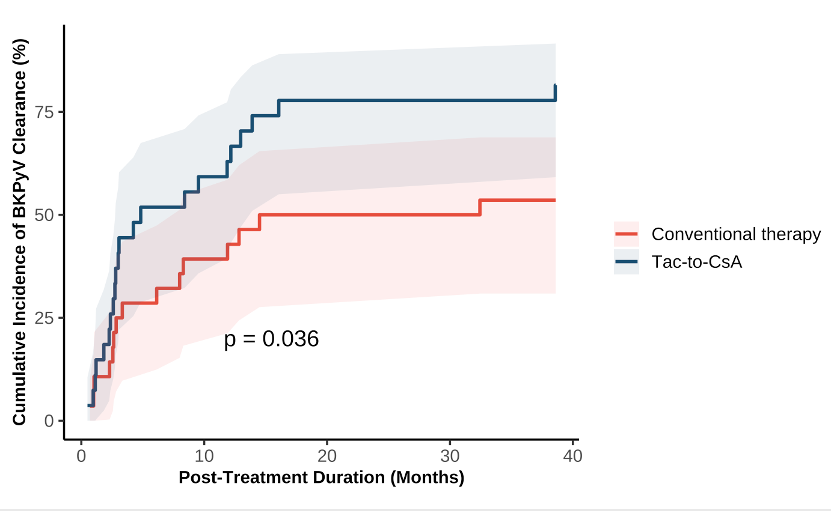
No significant differences were observed between the two groups in terms of panel-reactive antibody positivity (27.3% vs. 22.6%, p = 0.62) or incidence of acute rejection episodes (6.1% vs. 9.4%, p = 0.70).
Conclusions: High-level BK viruria is associated with inferior long-term graft outcomes and a heightened risk of BKPyVAN in pediatric kidney transplant recipients. Recipient age <5 years, donor age ≥5 years, and obstructive uropathy are key risk factors. Switching from tacrolimus to cyclosporine A appears to be a safe and effective strategy for preventing BKPyVAN progression and promoting viral clearance without increasing the risk of rejection in pediatric kidney transplant recipients.
References:
[1] BK Virus Infection
[2] Pediatric
[3] Kidney Transplant
[4] Tacrolimus to Cyclosporine A
Lectures by Jianming Li
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Sat-20 10:00 - 11:00 |
Infections and vaccines | Clinical Outcomes of Switching from Tacrolimus to Cyclosporine A in Pediatric Kidney Transplant Recipients with BK Virus Infection | MOA 5 |
