Rima S. Zahr DO, MS, United States
Associate Professor
Pediatric Nephrology and Hypertension
University of Tennessee Health Science Center
Kidney outcomes after hematopoietic cell transplantation in children and young adults with sickle cell disease
Rima Zahr1, Yu Bi2, Subodh Selukar2, Stephen Gottschalk3, Brandon M Triplett3, Alexis K Leonard 4, Akshay Sharma3.
1Pediatric Nephrology and Hypertension, University of Tennessee Health Science Center, Memphis, TN, United States; 2Biostatistics, St. Jude Children's Research Hospital, Memphis, TN, United States; 3Bone Marrow Transplantation and Cellular Therpay, St. Jude Children's Research Hospital, Memphis, TN, United States; 4Hematology, St. Jude Children's Research Hospital, Memphis, TN, United States
Kidney damage in children with sickle cell disease (SCD) begins in the first decade of life with development of chronic kidney disease (CKD). CKD contributes to early development of end stage kidney disease and early death in SCD. Hematopoietic cell transplantation (HCT) serves as a potentially curative therapy for patients with SCD with the possibility of stabilization or improvement in end organ function, however conditioning and other transplant therapies can be nephrotoxic. We sought to 1) assess the prevalence of acute kidney injury (AKI) in the hrst 48 hrs and 7 days after HCT, 2) determine kidney function at baseline, 1-, 6-, 12- and 24-months after HCT, 3) assess the prevalence of hyperfiltration defined by an eGFR > 135 mL/min/1.73m2, and 4) assess prevalence of chronic kidney disease after HCT by an estimated glomerular filtration rate (eGFR) < 90 mL/min/1.73m2.
Children and young adults with SCD received either a matched sibling donor (MSD) or a haploidentical donor (HAPLO) HCT following a reduced toxicity conditioning with alemtuzumab, thiotepa and low dose total body irradiation (NCT04362293). Patients were receiving either hydroxyurea or chronic transfusion therapy before HCT. All patients received a fresh apheresis derived peripheral blood hematopoietic cell graft. Sirolimus was used for graft versus host disease prophylaxis for 6-12 months post-HCT, with additional post-transplant cyclophosphamide for HAPLO recipients. The prevalence of AKI was assessed in the first 48hrs and 7 days post-HCT using the 2012 Kidney Disease Improving Global Outcomes clinical practice guideline. Kidney function was determined at baseline, 1-, 6-, 12- and 24-months after HCT by calculating eGFR using the bedside Schwartz formula.
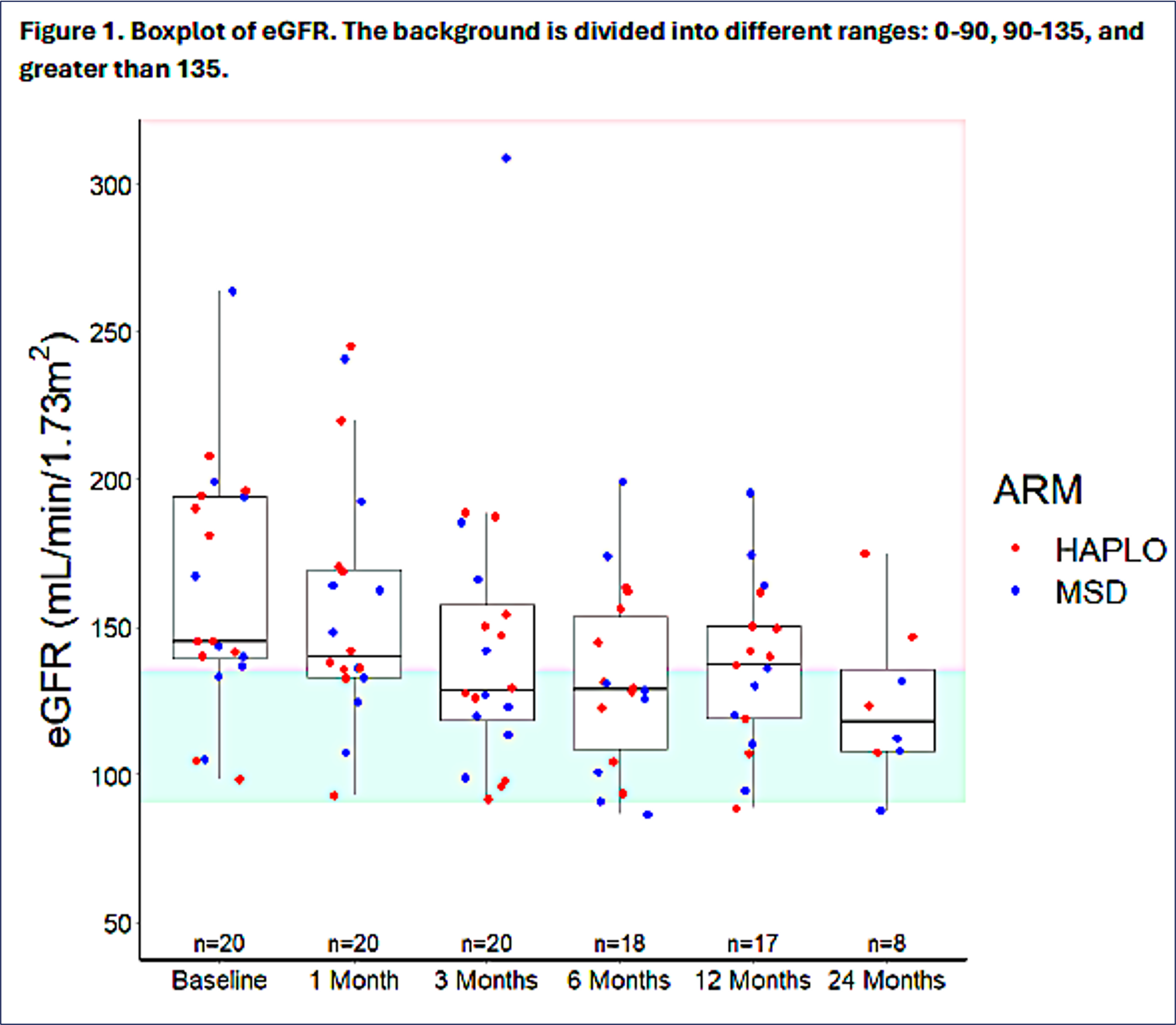
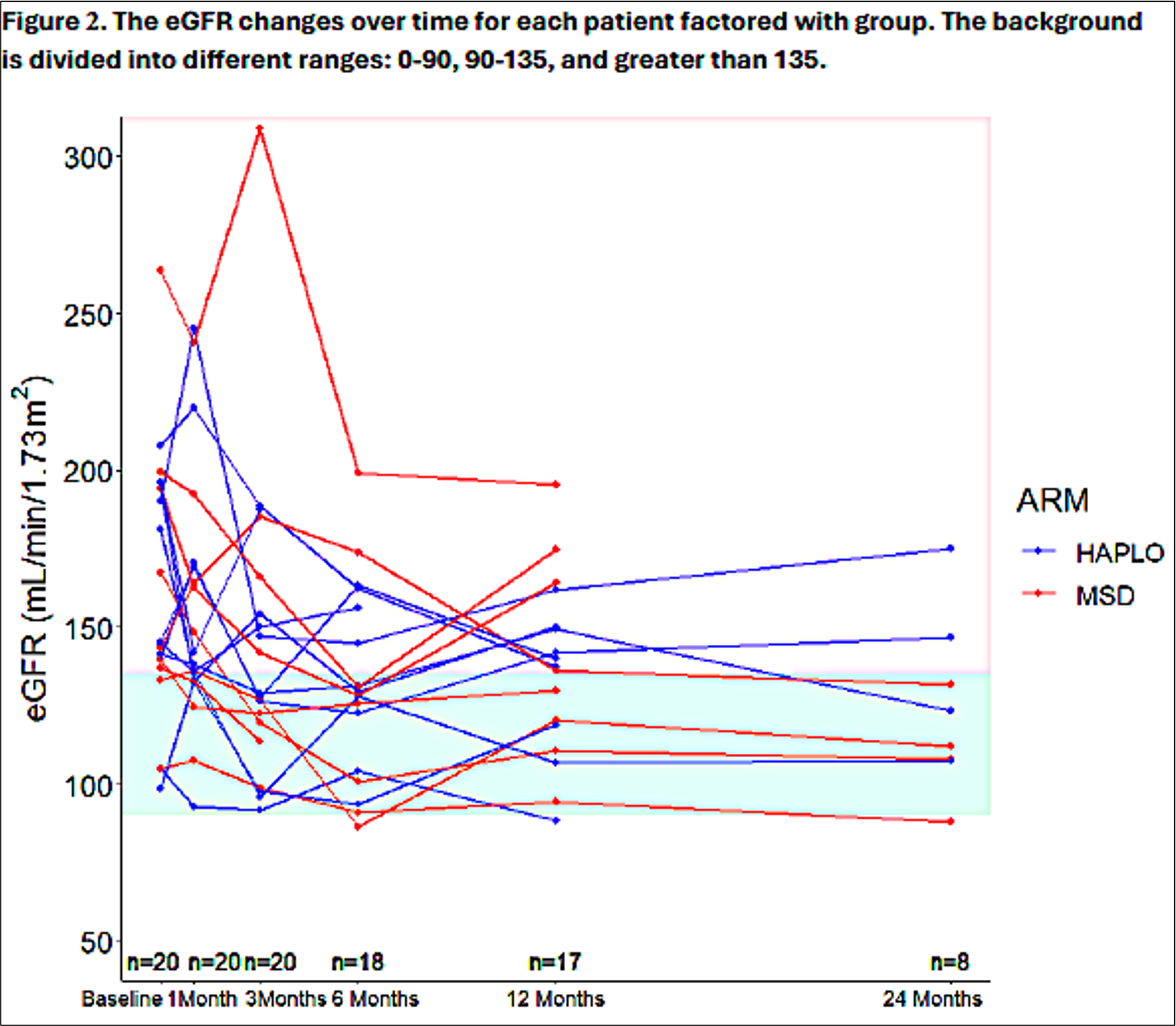
Twenty patients with SCD underwent HCT of which 11 received HAPLO HCT and 9 received MSD HCT. Participants were majority male (60%) with a median age of 15.3 years (6.5-23.5 years) at time of HCT. All patients engrafted and had expected HCT related acute toxicities. AKI was not observed in the first 48 hrs or 7 days after the cellular infusion in any participant. At baseline, median eGFR was 145 [98.5-264] mL/min/1.73m2 and decreased to 129 [86.5-199] mL/min/1.73m2 by 6 months. The median eGFR at 12-months was 137 [88.5-195] mL/min/1.73m2. The prevalence of hyperfiltration decreased from baseline, with 80% (16/20) at baseline versus 33.33% (6/18) at 6 months and 58.82% (10/17) at 1 year. With 8 patients having 2-year follow-up, the median eGFR at 2 years after HCT was 118 mL/min/1.73m2 with only a 25% (2/8) prevalence of hyperhltration. At baseline there was no evidence of CKD, with a 2-year prevalence of 12.5% (1/8).
Reduced toxicity conditioning HCT regimen is not associated with AKI early after HCT. CKD compromised a small percent of our population and long-term kidney function stabilized with decrease in prevalence of hyperfiltration. These findings need to be confirmed in a larger SCD HCT patient cohort.
References:
[1] Bone Marrow Transplant
[2] Kidney Outcomes
[3] Sickle Cell Disease
Lectures by Rima S. Zahr DO, MS
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Sat-20 10:00 - 11:00 |
Special topics in transplantation | Kidney outcomes after hematopoietic cell transplantation in children and young adults with sickle cell disease | MOA 3 |
