Dorota Broniszczak-Czyszek, Poland
Attending doctor
Department of Pediatric Surgery and Organ Transplantation
Children's Memorial Health Institute
The long-term outcome of kidney transplantation in pediatric patients with urinary tract dysfunction and a comparison of different methods of urinary outflow in children with lower urinary tract dysfunction in a single-centre experience
Dorota Broniszczak-Czyszek1, Katarzyna Pankowska-Woźniak1, Hor Ismail1, Rubik Jacek2, Wioletta Jarmużek2, Marek Szymczak1, Marek Stefanowicz1, Małgorzata Syczewska1, Piotr Gastoł3, Karina Felberg3, Piotr Kaliciński1.
1Department of Pediatric Surgery and Organ Transplantation, Children's Memorial Health Institute, Warsaw, Poland; 2Department of Nephrology, Kidney Transplantation and Hypertension, Children's Memorial Health Institute, Warsaw, Poland; 3Department of Urology, Children's Memorial Health Institute, Warsaw, Poland
Introduction: The study aimed to analyse the results of kidney transplantation (KTx) in patients with lower urinary tract dysfunction (LUTD) who had urine drainage into the dysfunctional bladder or an ileal conduit and to compare these results with Ktx in recipients with normal bladder function.
Material and methods: Of the 788 transplants performed in pediatric patients between 2000 and 2020, 88 transplants were performed to an ileal conduit. Bricker (11%) - group B, 173 KTx to a dysfunctional bladder (22%) - group D, and 527 transplants to a healthy bladder (67%) - group N. We analysed the incidence of urological complications, urinary tract infections (UTIs), graft and patient survival over 10 years after KTx. Graft function was assessed at 1, 3, 5, and 10 years post-KTx based on creatinine concentration and glomerular filtration rate (GFR). Statistical significance was set at 0.05.
The incidence of urological complications was highest in group B at 20.5%, in group D - at 16.2%, and in group N - at 7.9% (chi² test p=0.0002). The incidence of vesicoureteral reflux (VUR) in group D was 9%, while in group N, it was 2.5% (chi² test, p = 0.0001). In group B, the main complications were related to the intestinal conduit (11%). UTIs were most common in group D (41.6%), followed by patients in group B (28.7%) and group N (10%) (chi² test, p < 0.0001).
Graft survival was 91.9% after 1 year, 86% after 5 years and 70.3% after 10 years, respectively. Kaplan-Meier analysis of graft survival after 1, 5 and 10 years in groups B, D and N showed no statistically significant difference (p=0.564).
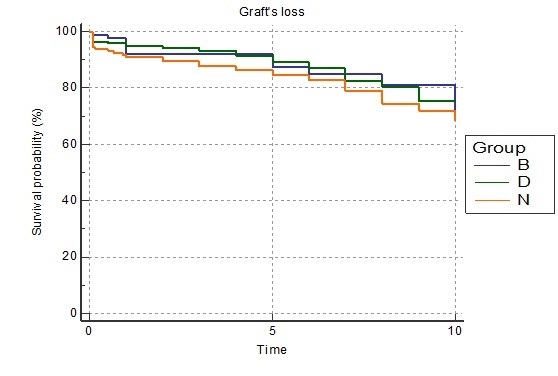
Patient survival rates were 98.8% at 1 year, 97.1% at 5 years, and 94.7% at 10 years, respectively. Kaplan-Meier analysis of patient survival after 1, 5, and 10 years in groups B, D, and N revealed no statistically significant difference (p = 0.95).
At 1 and 3 years after KTx, median creatinine concentrations in group B were significantly better than in groups D and N (p=0.005 and p=0.01, respectively). All groups showed no differences in median creatinine concentrations 5 years and 10 years after KTx. Evaluation of graft function revealed no difference in GFR at 1 and 3 years after KTx. However, 5 years after KTx in group D, GFR is significantly lower compared to groups B and N (75 vs 62.9 vs 68.4 for groups B, D, and N, respectively; p = 0.0479). Additionally, 10 years after transplantation, GFR in group D is lower compared to groups B and N (59.1 vs. 48.9 vs. 64.8 for groups B, D, and N, respectively; p = 0.0589).
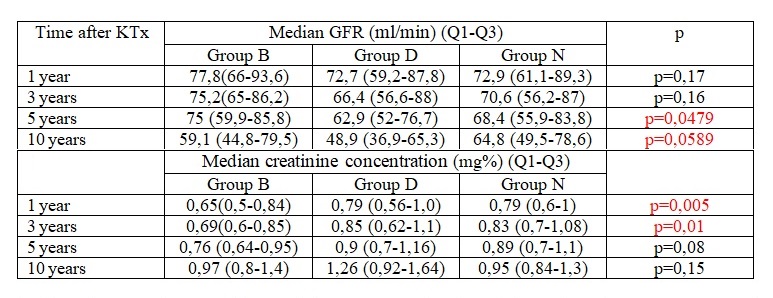
Conclusions: Urological complications and UTIs are most common in children with LUTD. Graft and patient survival do not show differences related to the mode of urinary diversion or the presence of LUTD over a 10-year follow-up period. Graft function in children after KTx into their dysfunctional bladder systematically deteriorates compared to transplants into a normal bladder or ileal conduit.
