Impact of HLA-DQα05 heterodimer mismatch on de novo donor-specific antibody formation in pediatric kidney transplantation
Vaka Sigurjonsdottir1, Kim Piburn 2, Daniel Turudic 3, Paul Grimm4, Anat Tambur5, Bing Zang4.
1University of Miami Miller School of Medicine,, Miami, FL, United States; 2The University of Texas Health Science Center at San Antonio, San Antonio, TX, United States; 3University Hospital Centre Zagreb, Zagreb, Zagreb, Croatia; 4Stanford University , Palo Alto, CA, United States; 5Northwestern University Feinberg School of Medicine, Chicago, IL, United States
Background: Recently, mismatches at the HLA-DQα/β heterodimer level have been recognized as important in transplant immunologic risk. In particular, donor heterodimers containing the DQα05 chain appear to be associated with a higher risk of developing de novo donor-specific antibodies (dnDSA).
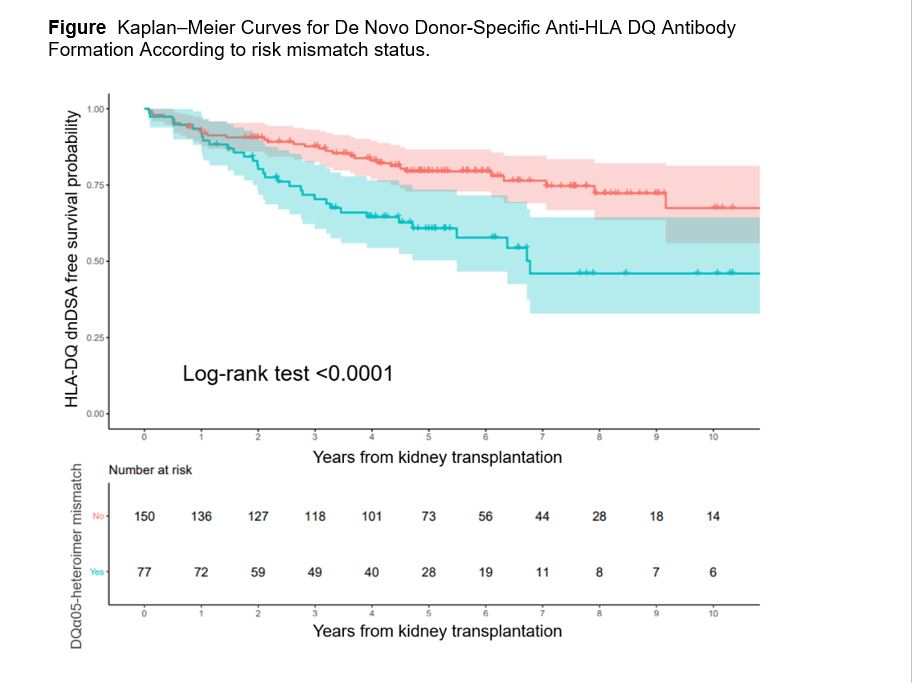
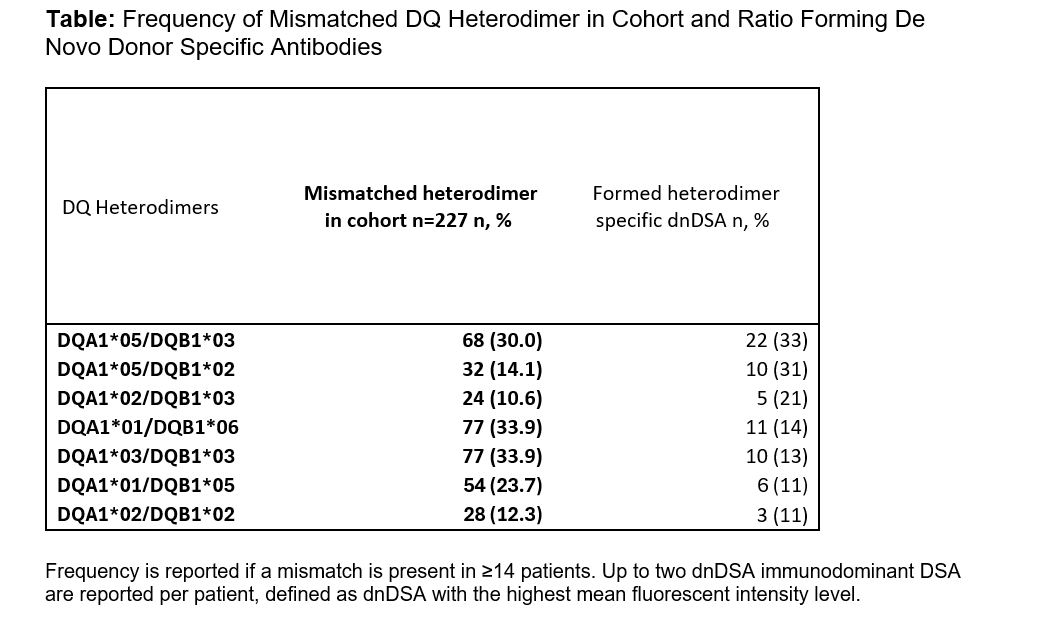
Methods: This retrospective cohort study included 227 pediatric kidney transplant recipients at Stanford Children’s Health (2010–2018) with ≥12-month follow-up through September 2022. HLA-DQ heterodimers were paired by linkage disequilibrium with DRB1 alleles. A DQα05 mismatch was defined when the donor expressed a DQα05-containing heterodimer not present in the recipient. dnDSA was defined as a post-transplant HLA-DQ antibody with MFI ≥3000 and absent pre-transplant. Antibody testing was performed at 0, 1, 2, 3, 6, 12 months, annually, and as clinically indicated. Kaplan-Meier survival and frequency analysis assessed the association between specific HLA-DQ heterodimer mismatches and dnDSA formation.
Results: A total of 227 patients were included (median age 14 years [IQR 4–17]; 49% female; 23% living donor). The median follow-up time was 73 months (IQR 58–96). 65/227 (28.6%) developed dnDSAs targeting HLA-DQ. Kaplan-Meier analysis showed that recipients with DQα05 mismatches were significantly more likely to develop dnDSA over time than those without DQα05 mismatches (p < 0.0001).
Mismatch frequency analysis demonstrated that specific heterodimer pairs were more commonly associated with dnDSA. The highest dnDSA formation rates were observed in recipients mismatched for DQA1*05/DQB1*03 (33%) and DQA1*05/DQB1*02 (31%), suggesting these specific DQα05 heterodimer mismatches may confer greater risk.
Conclusion: DQα05 heterodimer mismatch was strongly associated with the formation of HLA-DQ dnDSA in our cohort. Identifying DQ mismatches that carry a higher risk of dnDSA formation may help optimize allocation systems, guide organ selection for sensitized patients, and support immunologic risk stratification post-transplant to improve graft outcomes.
References:
[1] DSA (Donor-Specific Antibodies)
[2] HLA mismatch
[3] High-resolution typing
Lectures by Vaka K Sigurjonsdottir
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Sun-21 09:15 - 10:45 |
Monitoring after pediatric kidney transplant | Impact of HLA-DQα05 Heterodimer Mismatch on De Novo Donor-Specific Antibody Formation in Pediatric Kidney Transplantation | MOA 6 |
