Vice Chairman
Department of Pediatrics I
University Children's Hospital Heidelberg
Risk assessment of delayed graft function in pediatric kidney transplantation – A CERTAIN research network analysis
Christian Patry1, Miriam Boßung1, Manuel Feißt2, Kai Krupka1, Britta Höcker1, Lars Pape3, Nele Kanzelmeyer4, Lutz T Weber5, Jun Oh6, Atif Awan7, Thomas Simon8, Licia Peruzzi9, Ali Duzova10, Jon Jin Kim11, Mohan Shenoy12, Claus P Schmitt1, Alexander Fichtner1, Burkhard Tönshoff1.
1Department of Pediatrics I, Pediatric Nephrology, University Children’s Hospital, Heidelberg, Germany; 2Institute of Medical Biometry, University of Heidelberg, Heidelberg, Germany; 3Clinic for Paediatrics III, Essen University Hospital, Essen, Germany; 4Department of Pediatric Kidney, Liver and Metabolic Diseases, Hannover Medical School, Hannover, Germany; 5Pediatric Nephrology, Children’s and Adolescents’ Hospital, University Hospital Cologne, Medical Faculty University of Cologne, Cologne, Germany; 6Pediatric Nephrology, University Hospital Hamburg, Hamburg, Germany; 7Department of National Paediatric Renal Transplantation, Children's Health Ireland at Temple Street, Dublin, Ireland; 8Pediatric Nephrology, Toulouse University Hospital, Toulouse, France; 9Pediatric Nephrology Unit, Regina Margherita Children's Hospital, AOU Città della Salute e della Scienza di Torino, Torino, Italy; 10Division of Pediatric Nephrology, Hacettepe University Faculty of Medicine, Ankara, Turkey; 11Department of Paediatric Nephrology, Nottingham University Hospital, Nottingham, United Kingdom; 12Paediatric Nephrology, Royal Manchester Children's Hospital, Manchester, United Kingdom
CERTAIN Research Network. ESPN Transplantation Working Group.
Background: Delayed graft function (DGF) in pediatric kidney transplantation is a serious complication with a negative impact on patient and graft survival. It is primarily caused by ischemia-reperfusion injury in the immediate post-transplant period. Currently, there are no reliable methods available to assess the risk of DGF in children.
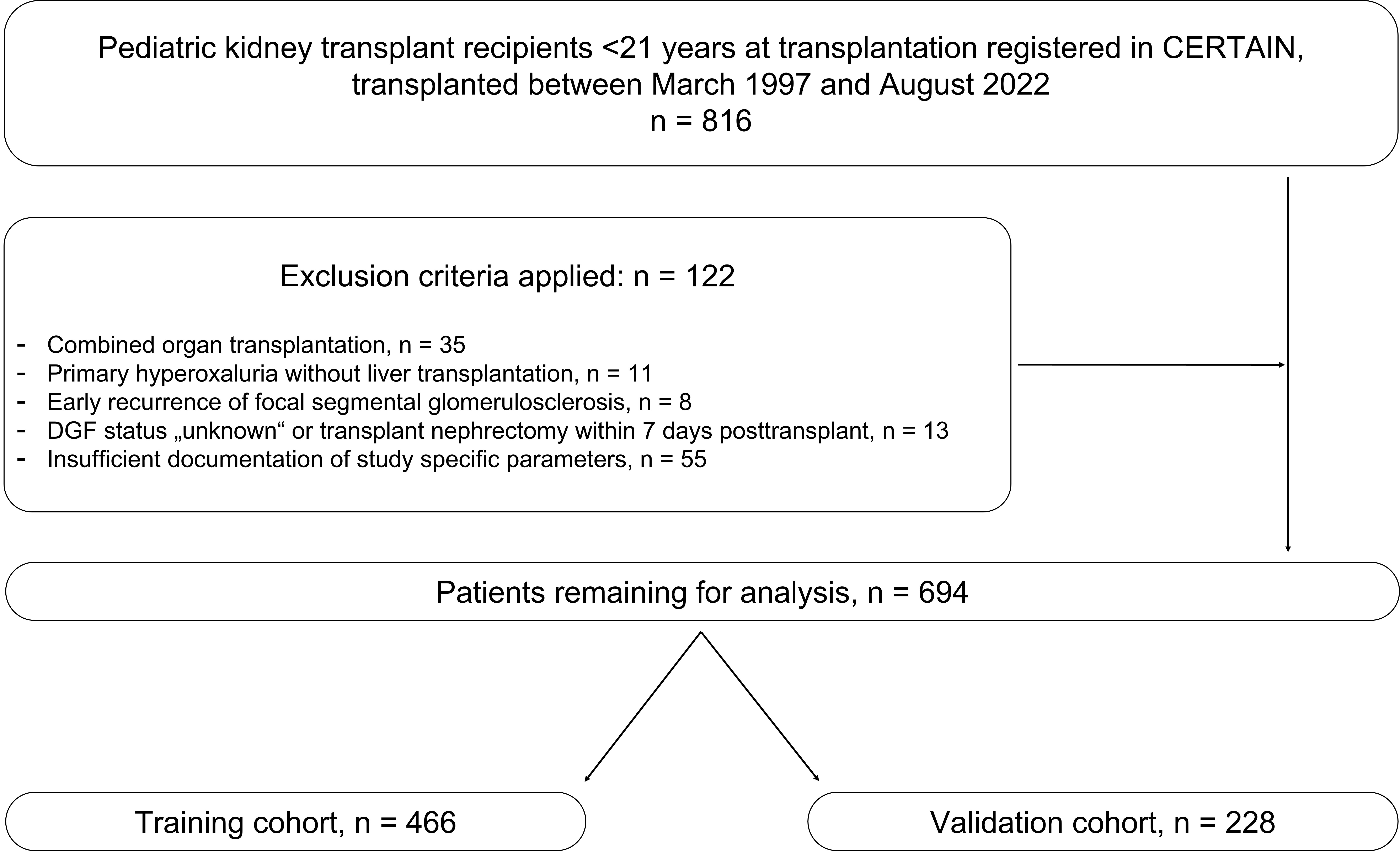
Methods: We performed a retrospective analysis of data from the Cooperative European Paediatric Renal Transplant Initiative (CERTAIN) registry to develop a specific DGF risk assessment model for pediatric kidney transplantation, based on recipient clinical and biochemical parameters associated with ischemia-reperfusion injury and available within the first 24 hours post-transplant. Patients were randomly assigned in a 2:1 ratio to a training and a test cohort.
The model was developed using multiple logistic regression with forward variable selection, supported by multiple imputation for missing data. Internal validation included both complete and imputed datasets. To control for interdependence of model parameters and to provide transparency, adjusted odds ratios were also calculated for each selected parameter in the model. In an extended analysis, we additionally explored whether selected pre-transplant parameters (pre-transplant dialysis mode, donor type, donor sex, recipient age, cold ischemia time, donor hemodynamic instability and number of HLA-DR mismatches) could enhance the model’s predictive performance.
Results: This study included 694 pediatric kidney transplant recipients. The overall DGF rate was 8.5%. The following four key post-transplant parameters were selected for the DGF risk assessment model: (i) occurrence of surgical complications requiring reoperation, (ii) immediate graft urine production, (iii) rate of change in recipient’s serum creatinine, and (iv) initial calcineurin inhibitor therapy. The model showed robust performance, with a ROC-AUC of 0.9043 in the training cohort and 0.878 in the validation cohort without imputed data. The model showed a relatively good performance in terms of calibration.
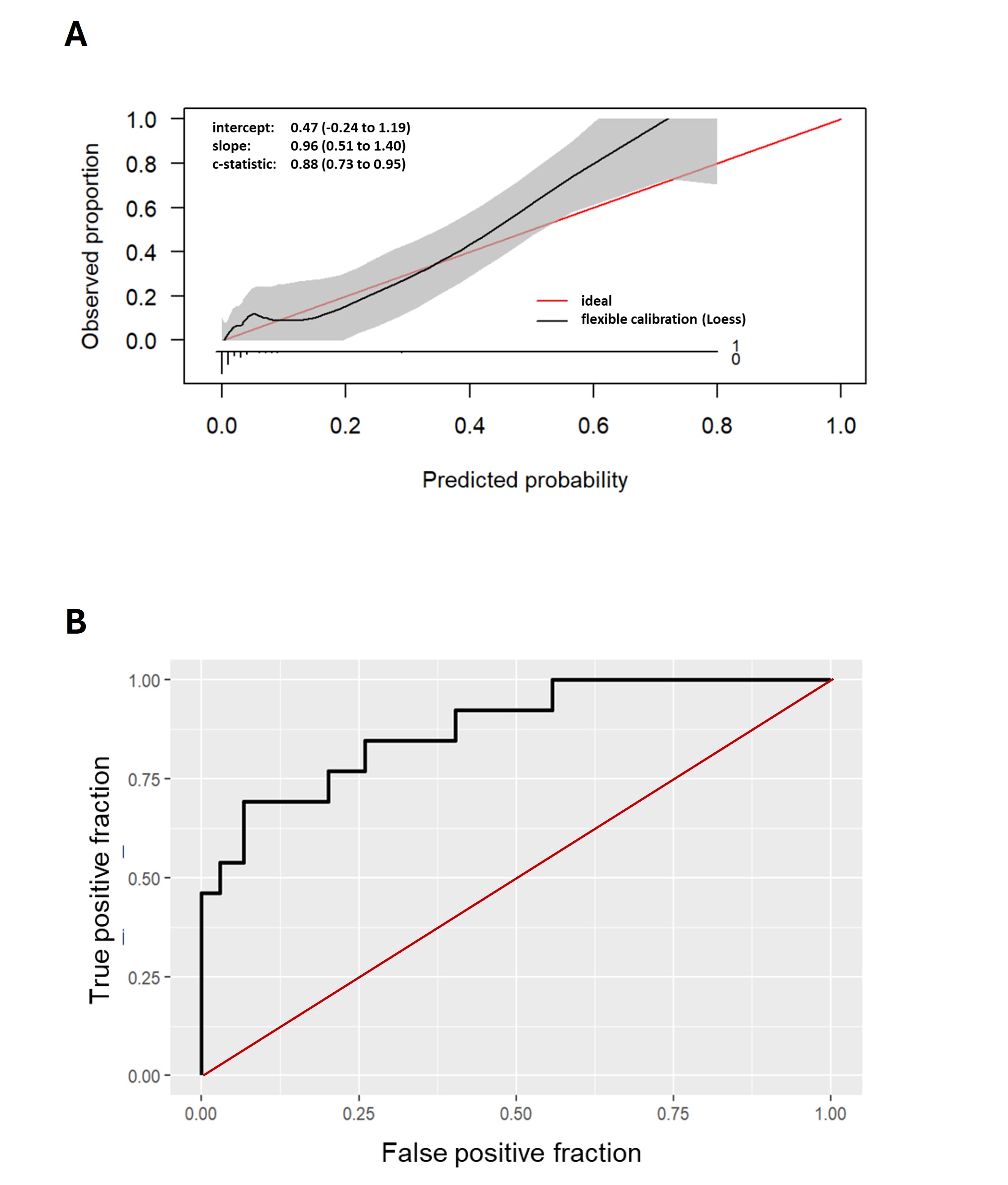
In the extended analysis, the inclusion of selected pre-transplant factors did not improve the model’s predictive accuracy. Only the number of HLA-DR mismatches was retained as a parameter in the combined model. However, this parameters contribution to the combined pre- and post-transplant model was marginal and it did not enhance the ROC-AUC (0.878) beyond the performance of the post-transplant model alone.
Conclusions: This multivariable model based on early post-transplant parameters can predict the occurrence of DGF in pediatric kidney transplant recipients with high accuracy. The reliable identification of patients at high risk for DGF may support individualized post-transplant care by aiding clinical decision-making in the immediate postoperative period and it may facilitate future interventional trials targeting ischemia-reperfusion injury in children.
References:
[1] Renal Transplantation
[2] Delayed Graft Function
[3] Risk Prediction Model
Lectures by Burkhard Toenshoff
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Fri-19 11:05 - 12:05 |
Histocompatibility | Tailoring HLA antibody monitoring post transplantation | MOA 6 |
|
Sun-21 07:00 - 07:50 |
Kidney transplantation | Risk assessment of delayed graft function in pediatric kidney transplantation – A CERTAIN research network analysis | MOA 4 |
|
Sun-21 09:15 - 10:45 |
Insights in immunology and immunosuppression | Association of intraindividual tacrolimus variability and concentration-to-dose ratio with allograft rejection in pediatric kidney transplant recipients | MOA 4 |
|
Fri-19 10:00 - 11:00 |
Adventures with immunosuppression | Unraveling interindividual differences and functional consequences of gut microbial metabolism of immunosuppressants | MOA 5 |
