Sonya R Kowalczyk, United States
Fellow Physiican
Division of Pediatric Nephrology
Children's Hospital of Philadelphia
Surveillance of post-transplant lymphoproliferative disorder in pediatric solid organ transplant recipients
Kaitlin J Devine2, Sonya Kowalczyk1, Jordyn Horan7, Kathleen Anderer3, Sandra Amaral1, Hamid Bassiri4, Carley Boyle5, Rachel Goldberg3, Maanasi Gothoskar2, Dimitrije Ibrocic7, Leah J Mita6, Anne F Reilly2, Alix E Seif2, Benjamin L Laskin1.
1Division of Nephrology, Children's Hospital of Philadelphia, Philadelphia, PA, United States; 2Division of Oncology, Children's Hospital of Philadelphia, Philadelphia, PA, United States; 3Division of Gastroenterology, Children's Hospital of Philadelphia, Philadelphia, PA, United States; 4Division of Infectious Disease, Children's Hospital of Philadelphia, Philadelphia, PA, United States; 5Division of Cardiology, Children's Hospital of Philadelphia, Philadelphia, PA, United States; 6Division of Pulmonary and Sleep Medicine, Children's Hospital of Philadelphia, Philadelphia, PA, United States; 7Transplant Center Program, Children's Hospital of Philadelphia, Philadelphia, PA, United States
Introduction: Post-transplant lymphoproliferative disorder (PTLD) is a neoplastic complication of solid organ transplantation (SOT). Recipient Epstein Barr virus (EBV) seronegativity is a known PTLD risk factor. Although screening for EBV viremia is routine, there is limited data to guide actions once EBV viremia occurs and there are no EBV-specific prophylactic or therapeutic medications. Data is needed to guide EBV monitoring and inform when EBV viremia warrants PTLD evaluation. Serial measurements of EBV levels in patients at highest risk for PTLD could allow for earlier immunosuppression reduction to prevent PTLD and earlier PTLD detection and treatment. We describe the results of the approach to EBV surveillance implemented at the Children’s Hospital of Philadelphia (CHOP).
Methods: A multidisciplinary committee of CHOP providers in hepatology, nephrology, cardiology, pulmonology, infectious disease, and oncology formed in 2017 to monitor patients after SOT for PTLD. Patients with standard risk of PTLD have EBV PCR testing every three months and patients with higher PTLD risk are monitored more closely at discretion of the primary team.
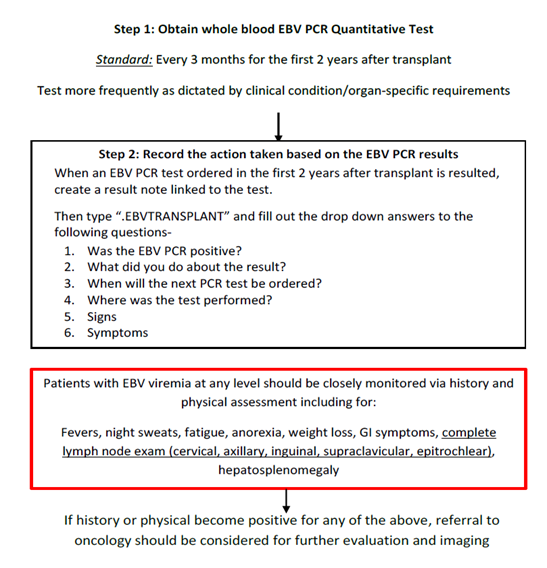
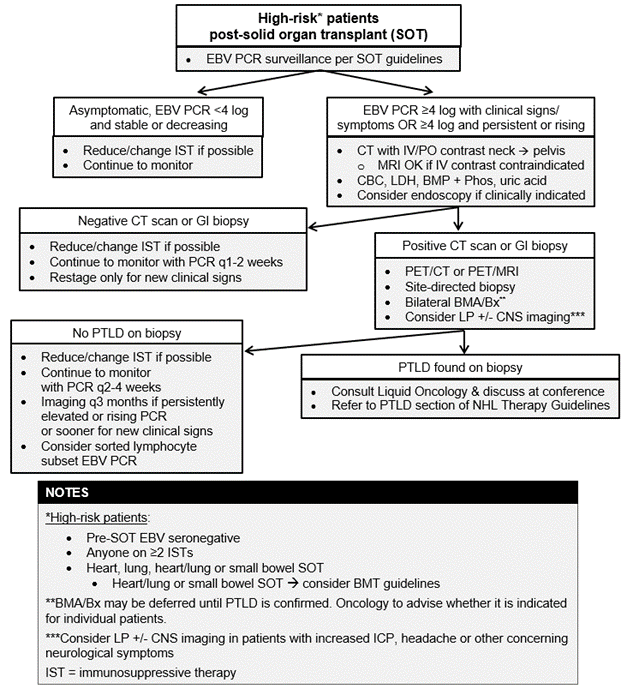
The multidisciplinary group meets monthly to discuss patients with new or rising EBV viremia to ensure immunosuppression is at the lowest acceptable level with greater focus on patients with EBV PCR ≥4.0 log IU/mL. Patients are closely monitored for PTLD symptoms with referral to oncology if symptoms arise or if EBV persists ≥ 4.0 log IU/mL. Notes are entered into patient records documenting EBV level, signs/ symptoms, interventions, and next EBV level.
Results: From January 1, 2017 through June 1, 2024, 347 patients received SOT at CHOP and were included in the EBV surveillance program. 107 (30.8%) of patients were EBV positive. 29 patients (8.4%) developed PTLD. Of patients diagnosed with PTLD, there were 21 liver (72.4%), 4 kidney (13.7%), 2 heart (6.9%), 1 lung (3.4%), and 1 liver/kidney (3.4%) transplant recipients. 27 patients (93.1%) were symptomatic. 18 patients (62.1%) were EBV sero-negative prior to transplant and 25 (86.2%) had EBV PCR ≥4.0 log IU/mL prior to diagnosis. 16 patients (55.2%) had nondestructive disease, 6 patients (20.6%) had monomorphic disease, and 7 patients (24.1%) had polymorphic disease. 2 patients (6.9%) died, but neither from PTLD. The median follow-up was 30 months (3-78) with 30-month overall survival 96% (95% CI 74.8, 99.4) and 30-month relapse-free survival 86.3% (95% CI 61.9, 95.6).
Conclusion: EBV-negative serostatus prior to SOT and EBV viremia are known risk factors for PTLD. The surveillance algorithm developed at CHOP includes protocolized monitoring of EBV levels with increased monitoring of high-risk patients. Multidisciplinary collaboration created a unique surveillance approach with the aim of earlier diagnoses and improved outcomes. This approach needs further study to evaluate its impact on PTLD outcomes and survival.
Nicholas Cipriano Fund.
References:
[1] Post-Transplant Lymphoproliferative Disease
[2] Solid Organ Transplant
[3] Ebstein-Barr Virus (EBV)
[4] Surveillance
[5] Immunosuppression
[6] Detection
[7] Liver Transplant
[8] Lung Transplant
[9] Renal Transplant
[10] Heart Transplant
Lectures by Sonya R Kowalczyk
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Fri-19 13:35 - 15:05 |
Breakthroughs not outbreaks - ID and PTLD | Surveillance of Post-Transplant Lymphoproliferative Disorder in Pediatric Solid Organ Transplant Recipients | MOA 3 |
