Longshan Liu, People's Republic of China
Chief Physician
Organ Transplant Center
The First Affiliated Hospital, Sun Yat-sen University
Impaired renal function at 1-year after for-cause biopsy affected long-term graft survival in pediatric kidney transplant recipients
Longshan Liu1, Jianming Li 1, Jinghong Tan1, Zicong Li1, Huanxi Zhang1, Chenglin Wu1, Qian Fu1, Jun Li1, Changxi Wang1.
1Organ Transplant Center, The First Affiliated Hospital, Sun Yat-sen University , Guangzhou , People's Republic of China
Objective: To analyze the pathological characteristics of for-cause biopsies in pediatric kidney transplant recipients and to identify clinical and pathological risk factors associated with long-term graft survival.
Methods: This was a retrospective study involving pediatric kidney transplant recipients who underwent for-cause allograft biopsy. Data on pathological scores, biopsy diagnoses, allograft function, and graft survival were collected. Impaired renal function (IRF) at one year post-biopsy was defined as a >20% decline in estimated glomerular filtration rate (eGFR) compared to the time of biopsy. Multivariate analysis was conducted to identify independent risk factors associated with poor graft outcomes.
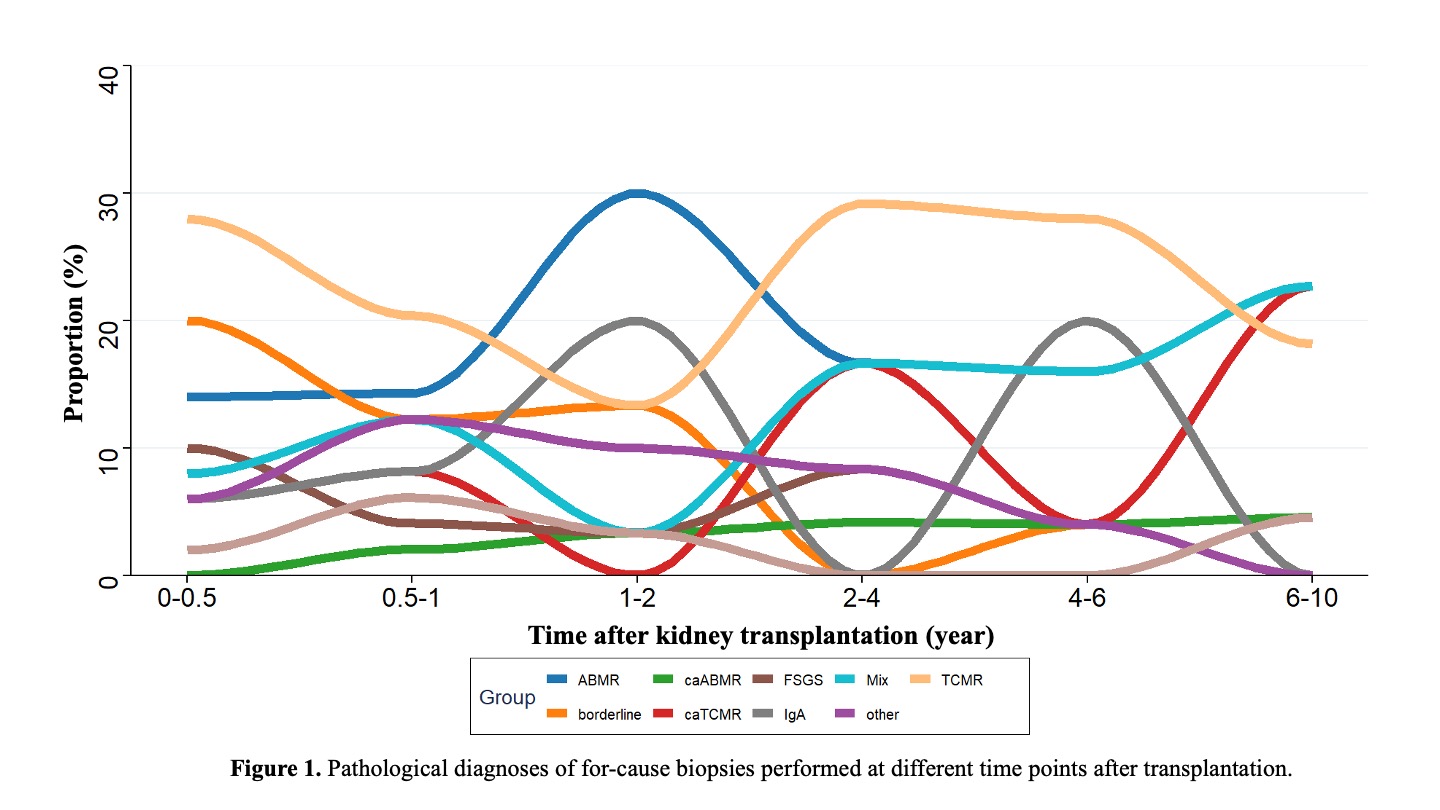
Results: Between March 2012 and May 2023, a total of 477 pediatric kidney transplants were performed at our center, of which 96 recipients who underwent for-cause biopsies were included in this study. A total of 136 biopsy episodes were analyzed. The pathological diagnoses included rejection (54.3%), recurrent or de novo transplant nephropathy (25.7%), BK virus nephropathy (3.6%), and others (16.4%). Among the rejection cases, 16.5% were borderline, 21.8% TCMR, 12.8% caTCMR, 27.1% ABMR, 3.8% caABMR, and 18% mixed rejection. Among glomerular diseases, IgA nephropathy accounted for 48.5%, FSGS for 33.3%, and others for 18.2%. Figure 1 illustrates the distribution of biopsy-proven pathological diagnoses at various time points post-transplantation.
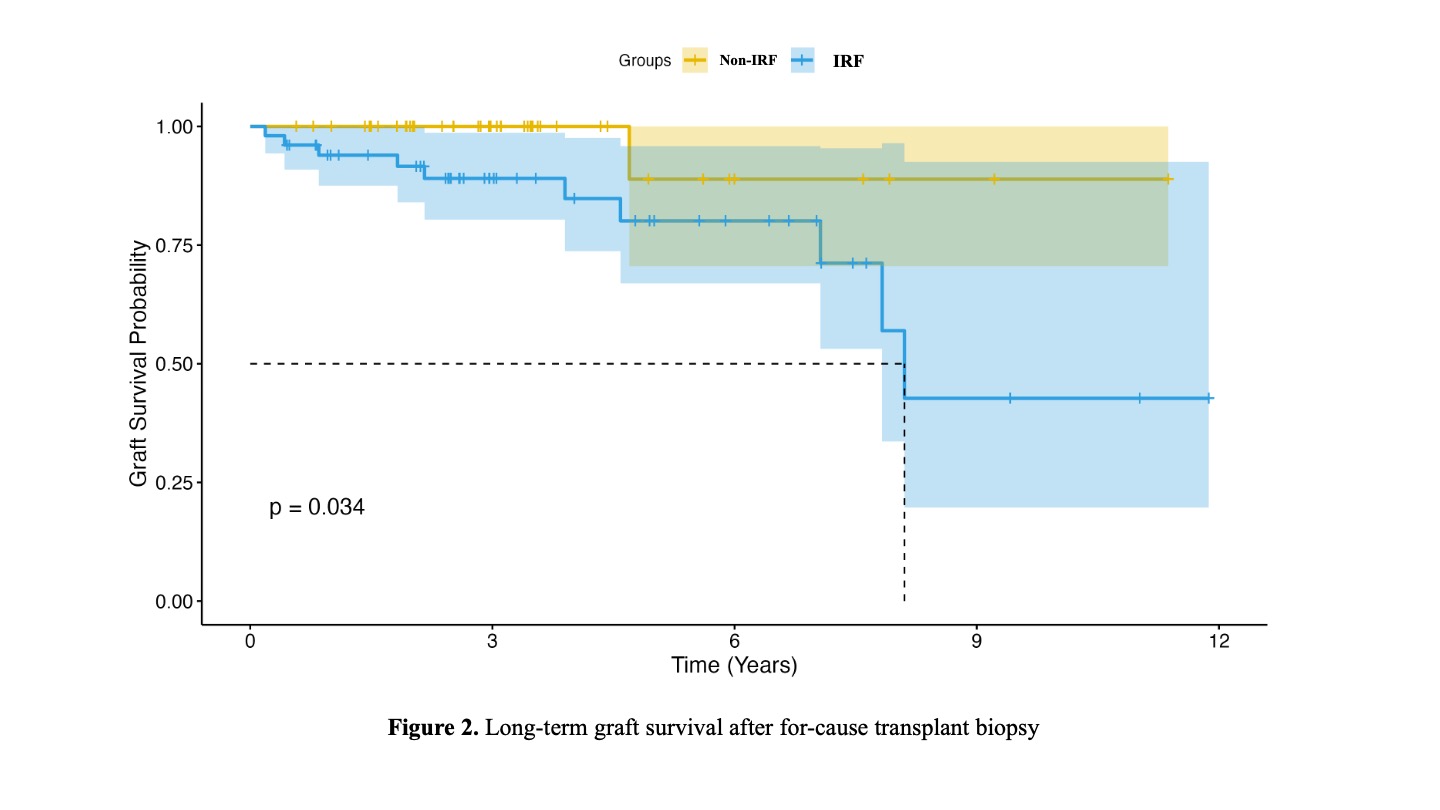
Based on graft function one year post-biopsy, patients were divided into the IRF group (n=51) and non-IRF group (n=45). The graft loss rate was significantly higher in the IRF group than in the non-IRF group (19.6% vs. 2.2%). Kaplan-Meier analysis showed a significantly reduced long-term graft survival in the IRF group (Figure 2). Multivariate analysis confirmed that IRF was an independent risk factor for late graft loss (OR=8.93, p=0.03). Further subgroup analysis revealed that the IRF group had higher proportions of TCMR (31.4% vs. 17.8%, p=0.194), caTCMR (23.5% vs. 6.7%, p=0.05), and mixed rejection (25.5% vs. 8.9%, p=0.06). Multivariate analysis revealed chronic active T cell–mediated rejection (caTCMR) (OR = 4.73, p = 0.02) and non-adherance (OR = 3.81, p = 0.05) were independent risk factors for the development of impaired renal function (IRF).
Conclusion: Rejection is the leading pathological finding in for-cause biopsies among pediatric kidney transplant recipients. Impaired renal function at one year after for-cause biopsy significantly contributes to long-term graft loss. Chronic active T cell–mediated rejection (caTCMR) is a key driver of persistent graft dysfunction and inferior long-term outcomes.
References:
[1] kidney transplantation
[2] transplant biopsy
[3] T-cell mediated rejection
[4] graft survival
[5] impaired renal function
