Tolerating unfavorable donor criteria in pediatric kidney transplantation: A retrospective UNOS analysis
Zachary Oatley1, Rupesh Raina2,3, Jieji Hu3, Jun Oh4, Priya S Verghese5.
1College of Medicine, Northeast Ohio Medical University, Rootstown, OH, United States; 2Department of Pediatric Nephrology, Akron Children's Hospital, Akron, OH, United States; 3Department of Nephrology, Akron Nephrology Associates at Cleveland Clinic Akron General Medical Center, Akron, OH, United States; 4Department of Pediatric Nephrology, University Medical Center Hamburg/Eppendorf, Hamburg, Germany; 5Northwestern University, Feinberg School of Medicine , Chicago, IL, United States
Background: Pediatric kidney transplant supply far outpaces demand. One approach to this problem is to expand donor criteria without compromising recipient outcomes. Live-related donors (LRD) are known to offer superior outcomes compared to deceased donors (DD) but outcomes in suboptimal LRDs have not been studied.
Methods: In this retrospective review of primary kidney recipients <18 years in the United Network for Organ Sharing database that received ABO matched donor kidneys on or after 2010, 10-year graft survival of perfect DD recipients was compared to suboptimal LRD recipients with unfavorable risks like diabetes history, hypertension (treated with medication), smoking history (≥10 pack-years), BMI (≥30), HLA mismatch (≥3), creatinine (≥1.5mg/dL) and age (≥50 years). Graft survival was compared using the log-rank test and depicted graphically with a Kaplan-Meier curve.
Results: Perfect DDs comprised 2.9% (n=175) of DD (N=6,060), while suboptimal LRDs with 1 and 2-criteria made up 68% (n=1,575) and19.6% (n=455) of the overall LRD (N=2,315) respectively.
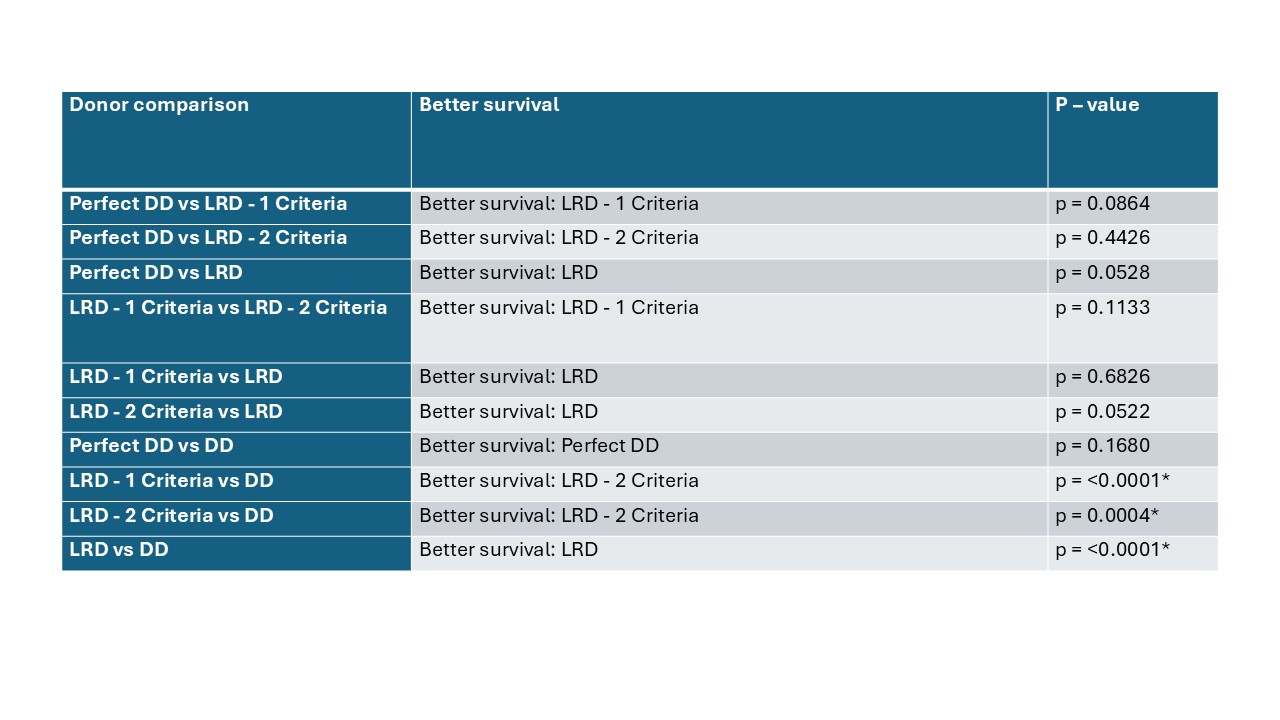
Perfect DDs had a mean 10-year graft survival of 0.725 (95% CI: 0.659 - 0.791). For overall LRD, with 1-criteria and with 2-criteria, the 10-year graft survival were 0.805 (0.789 - 0.821), 0.797 (0.777 - 0.816), and 0.746 (0.706 - 0.786), respectively. LRD groups had significantly superior graft survival compared to all DD groups, while perfect DD trended toward higher graft survival but was not superior to all DD groups [0.628 (0.616 - 0.640)] (p = 0.1680).
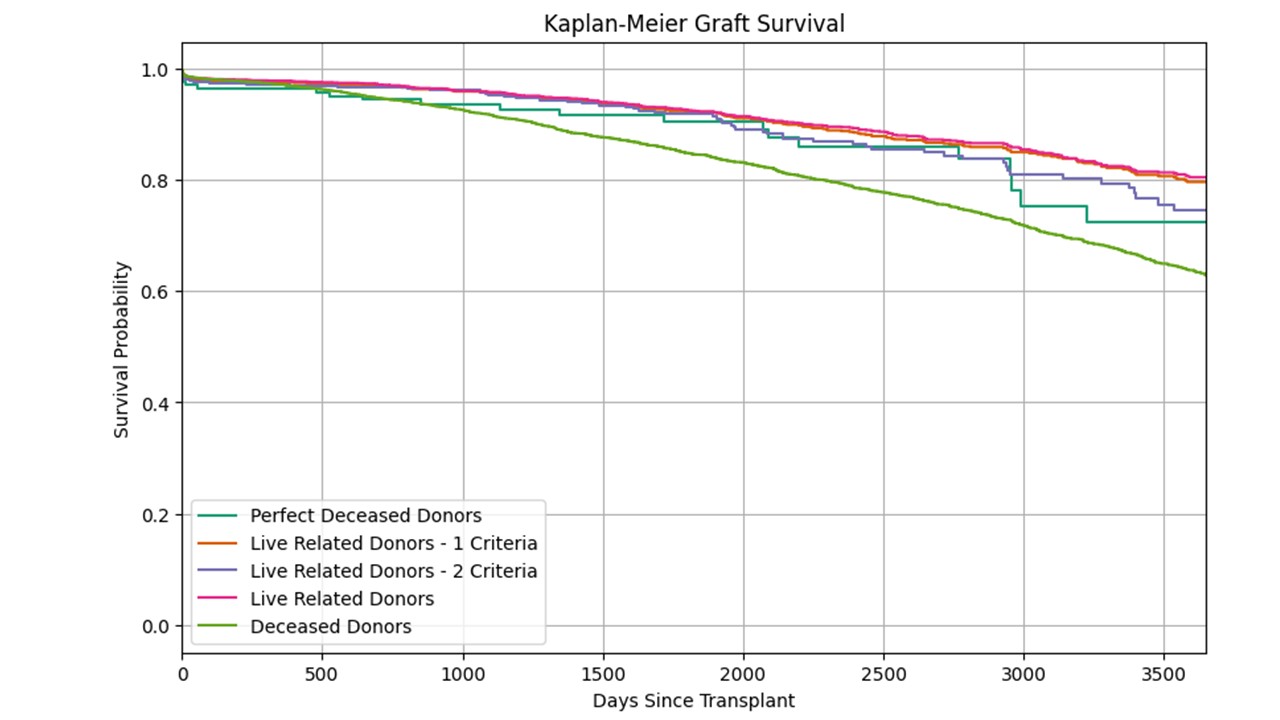
All the LRD groups achieved better, though not statistically significant, graft survival than perfect DD (p>0.05).
Conclusion: This preliminary analysis suggests that significant unfavourable criteria may be tolerated in LRD. Perfect DDs represent the most ideal scenario for a DD, with suboptimal LRD’s still achieving noninferior outcomes despite multiple unfavourable criteria. These data support a re-evaluation of donor selection and allocation policies to account for the tangible benefits—such as shortened wait times and better long-term outcomes—conferred by suboptimal live donation. Future prospective studies and risk stratification models will further refine donor selection criteria to improve the care of pediatric transplant recipients.
References:
[1] Allograft survival
[2] Kidney transplant
[3] Deceased donor
[4] Living donor
Lectures by Zachary Oatley
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Fri-19 13:35 - 15:05 |
Improving survival following pediatric kidney transplant | Tolerating Unfavorable Donor Criteria in Pediatric Kidney Transplantation: A Retrospective UNOS Analysis | MOA 6 |
|
Thu-18 17:00 - 18:00 |
Kidney Posters - from P1.1 to P1.32 | Evaluating Recurrent Glomerulonephritis in Kidney Transplantation | MOA 10 (Exhibit Area) |
