Ioannis A. Ziogas, United States
General Surgery Resident
Division of Transplant Surgery, Department of Surgery
University of Colorado Anschutz Medical Campus, Children's Hospital Colorado
Use of machine perfusion in pediatric liver transplantation
Ioannis Ziogas1, Emmanouil Giorgakis2, Dor Yoeli1, Maria Baimas-George1, Katie R. Conover3, Amy G. Feldman3, Varvara A. Kirchner4, Andrew S. Barbas5, Megan A. Adams1, Sarah A. Taylor3.
1Division of Transplant Surgery, Department of Surgery, University of Colorado Anschutz Medical Campus, Children's Hospital Colorado, Aurora, CO, United States; 2Division of Abdominal Transplantation, Department of Surgery, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC, United States; 3Department of Pediatrics, Pediatric Liver Center, University of Colorado Anschutz Medical Campus, Children's Hospital Colorado, Aurora, CO, United States; 4Division of Abdominal Transplantation, Department of Surgery, Stanford University School of Medicine, Palo Alto, CA, United States; 5Division of Abdominal Transplant Surgery, Department of Surgery, Duke University Medical Center, Durham, NC, United States
Introduction: Machine perfusion (MP) can be used for the assessment and preservation of marginal donor liver grafts to help expand the donor pool. When compared to static cold storage of donor organs, MP has been associated with reduced preservation-related graft injury and greater organ utilization. However, its use has been primarily limited to adult liver transplantation (LT) and its impact on pediatric LT has yet to be evaluated. We aimed to compare the characteristics and outcomes of children undergoing LT with vs without MP.
Methods: We retrospectively compared children (<18 years) undergoing first LT with vs without MP using the United Network for Organ Sharing database (01/01/2016-12/31/2024). The MP group was compared to all non-MP and to propensity score matched non-MP LT recipients. Propensity score matching was performed with 1:1 nearest neighbor matching using recipient age and sex, donor age, donation after circulatory death (DCD) status, and LT year as the matching variables with propensity scores estimated via logistic regression.
Results: Forty MP pediatric LT recipients were compared to 3,857 non-MP allcomers and 40 non-MP matched recipients. Thirty-seven children underwent normothermic MP (92.5%) and two hypothermic oxygenated MP (5.0%), while for one the type of MP was not available (2.5%). The percentage of pediatric LTs performed using MP significantly increased over time with only 0.2% MP use in 2016 versus 6.0% use in 2024 (rho 0.72, p = 0.03; Figure 1. 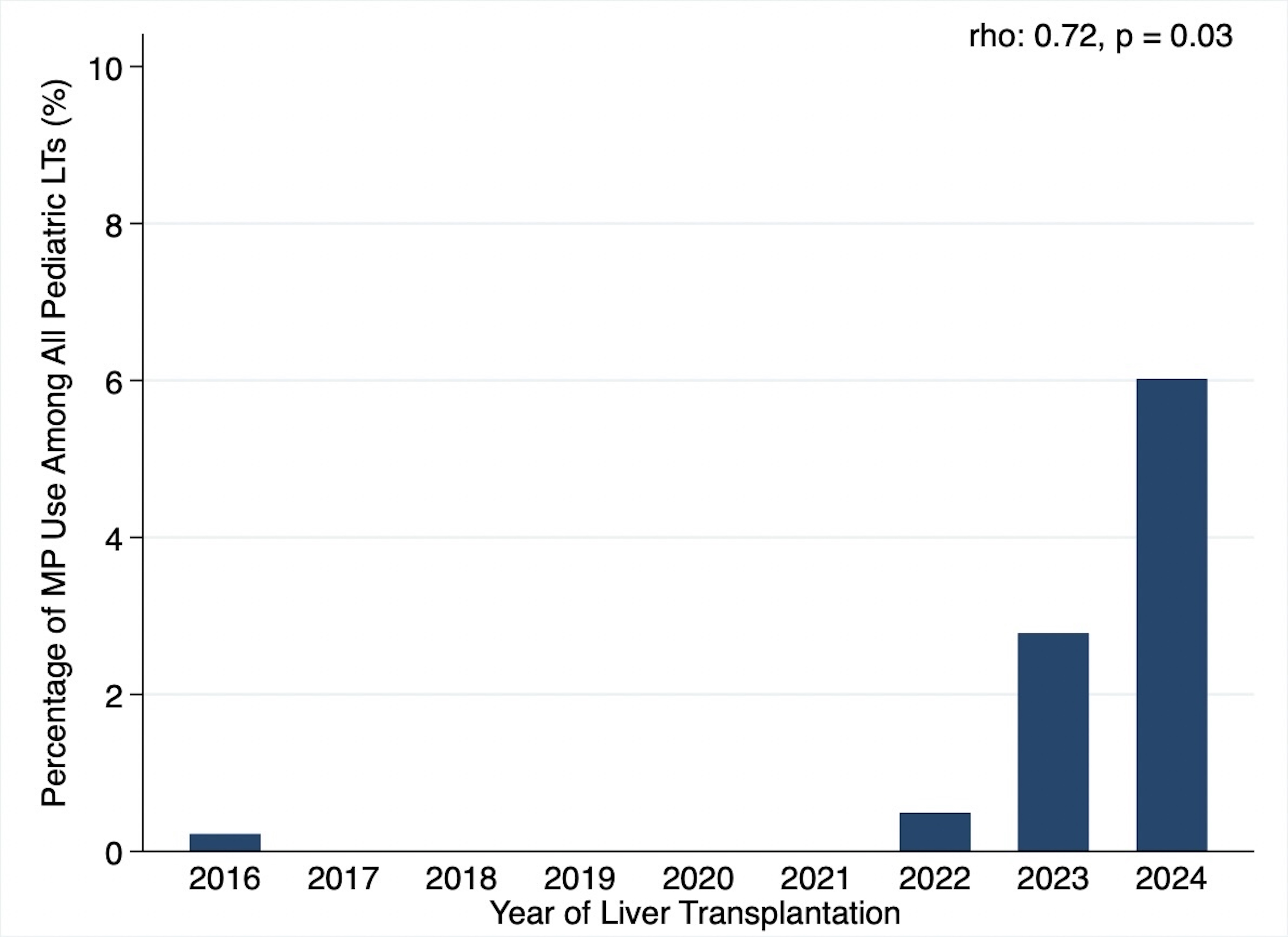
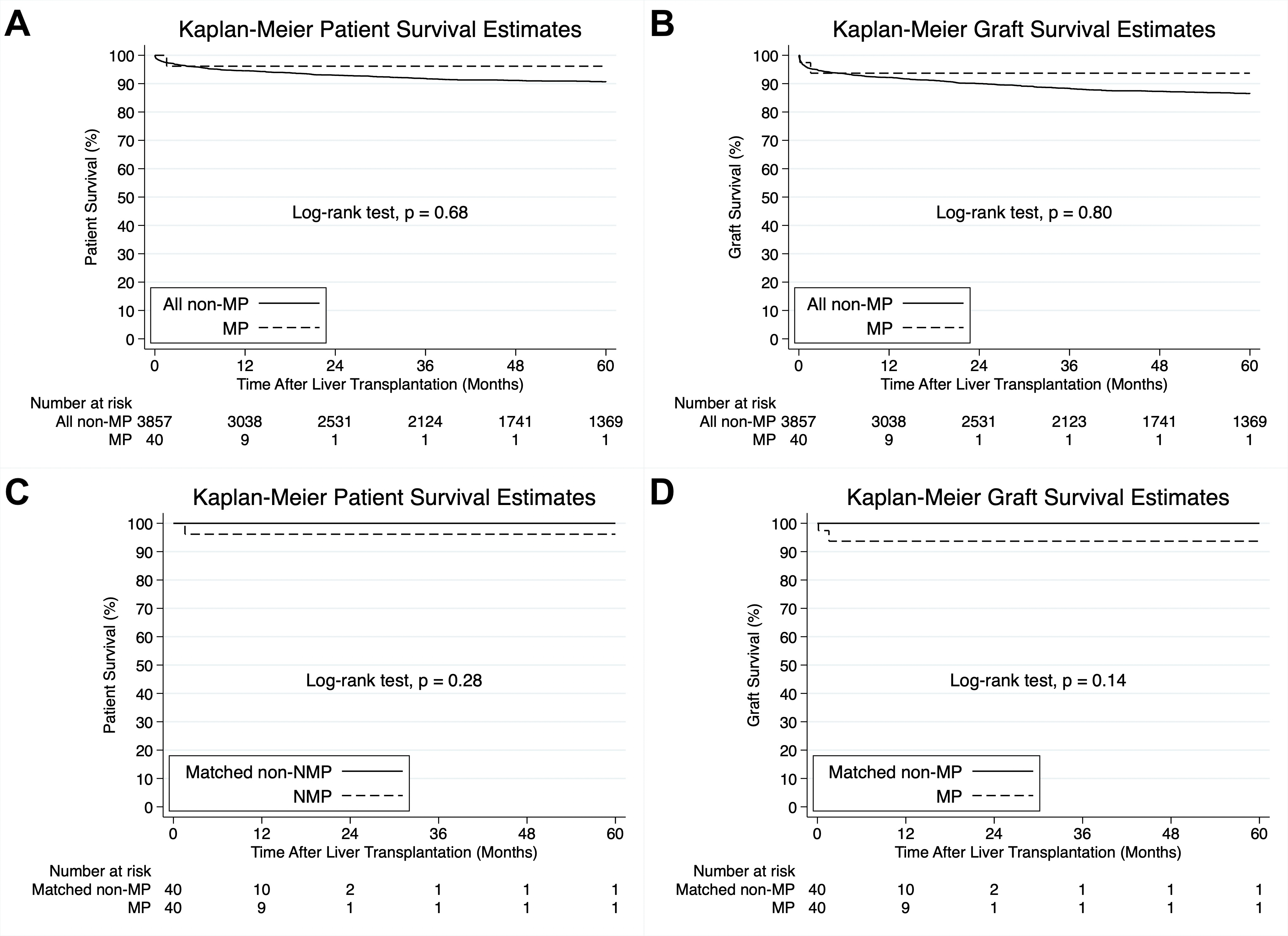
Compared to all non-MP patients, MP patients weighed more (median 31.8 vs 14.6 kg, p=0.047), were less likely to be White (27.5% vs 48.1%, p=0.01), had higher laboratory MELD/PELD score (median 16.5 vs 12.0, p=0.03), and were more likely to receive split grafts (42.5% vs 21.6%, p=0.001) allocated at a national level (65.0% vs 40.8%, p=0.007) from older donors (median 16.0 vs 11.0 years, p<0.001) with longer organ preservation time (median 15.0 vs 6.5 hours, p<0.001). Although not statistically different, DCD liver grafts were used in 20.0% of LTs in the MP group compared to 11.1% in the all non-MP group (p=0.08). Compared to matched non-MP recipients, MP recipients were more likely to have ascites (42.5% vs 15.0%, p=0.02) and had longer organ preservation time (median 15.0 vs 6.1 hours, p<0.001). There was no statistically significant difference regarding patient or graft survival between the MP and the all non-MP group (p=0.68 and p=0.80, respectively; Figure 2A-B) or the matched non-MP groups (p=0.28 and p=0.14, respectively; Figure 2C-D).
Conclusion: This initial US report of MP in pediatric LT demonstrates a significant increase in the use of MP in pediatric LT and the possibility of using MP to expand the donor pool by implementation of DCD or split grafts, while allowing for prolonged organ preservation times and national level allocation, without negatively impacting survival.
References:
[1] Machine perfusion
[2] Pediatric liver transplantation
[3] Deceased donation
[4] Donation after circulatory death
[5] Organ preservation
Lectures by Ioannis A. Ziogas
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Thu-18 16:00 - 17:00 |
Best Organ Preservation, Surgery and Immunosuppression Abstracts | Use of machine perfusion in pediatric liver transplantation | MOA 4 |
