HLA-DQ: The dominant driver of de novo donor-specific antibody-mediated graft failure in pediatric kidney transplantation
Daniel Turudic 1, Vaka Sigurjonsdottir2, Anat Tambur 3, Paul Grimm4, Bing Zhang 4.
1University of Zagreb , Zagreb, Croatia; 2University of Miami, Miami, FL, United States; 3Northwestern University , Chicago, IL, United States; 4Stanford University , Stanford, CA, United States
Background: De novo donor-specific antibodies (dnDSA) targeting HLA-DQ are increasingly recognized as the primary mediators of chronic antibody-mediated rejection and graft failure, yet their impact on pediatric kidney transplantation outcomes remains underappreciated.
Objective: This study aims to delineate the differential effects of HLA-DQ and HLA-DR dnDSAs on long-term graft survival.
Methods: This retrospective cohort study included pediatric kidney transplant recipients with at least 12 months of follow-up. The primary outcome was graft failure. Anti-HLA antibody testing was conducted pre-transplant and at 1, 2-, 3-, 6-, and 12-months post-transplant. dnDSA were defined as post-transplant mean fluorescence intensity (MFI) ≥3000 and absent pre-transplant. Complement-binding anti-HLA antibodies were tested using the C1q assay. Biopsies were scored per the latest Banff criteria. Kaplan-Meier curves and Cox proportional hazards models were used for survival analysis.
Results: 227 pediatric kidney transplant recipients were included (median age: 14 years, IQR: 4–17), with a median follow-up of 73 months (IQR: 58–96). HLA-DQ dnDSA were detected in 29% (65/227) of patients, compared to 16% (36/227) for HLA-DR dnDSA. 11% (25/227) formed both HLA-DQ and HLA-DR dnDSAs. Graft failure occurred in 47.62% of patients with both dnDSAs, 28.57% with HLA-DQ dnDSA alone, and none with isolated HLA-DR dnDSA. HLA-DQ dnDSA alone was a strong predictor of graft failure (HR: 4.74, 95% CI: 1.55–14.48, p=0.006), whereas HLA-DR dnDSA conferred lower risk (HR: 2.85, 95% CI: 1.09–7.48, p=0.033). However, the presence of both HLA-DQ and HLA-DR dnDSAs dramatically increased graft failure risk (HR: 7.83, 95% CI: 3.30–18.57, p<0.001), exceeding the sum of individual risks, suggesting a synergistic effect. C1q HLA-DQ dnDSA was strongly associated and preceded graft failure nearly a year, reinforcing its pathogenic role (52.4% vs. 16.0%, p=0.0004).
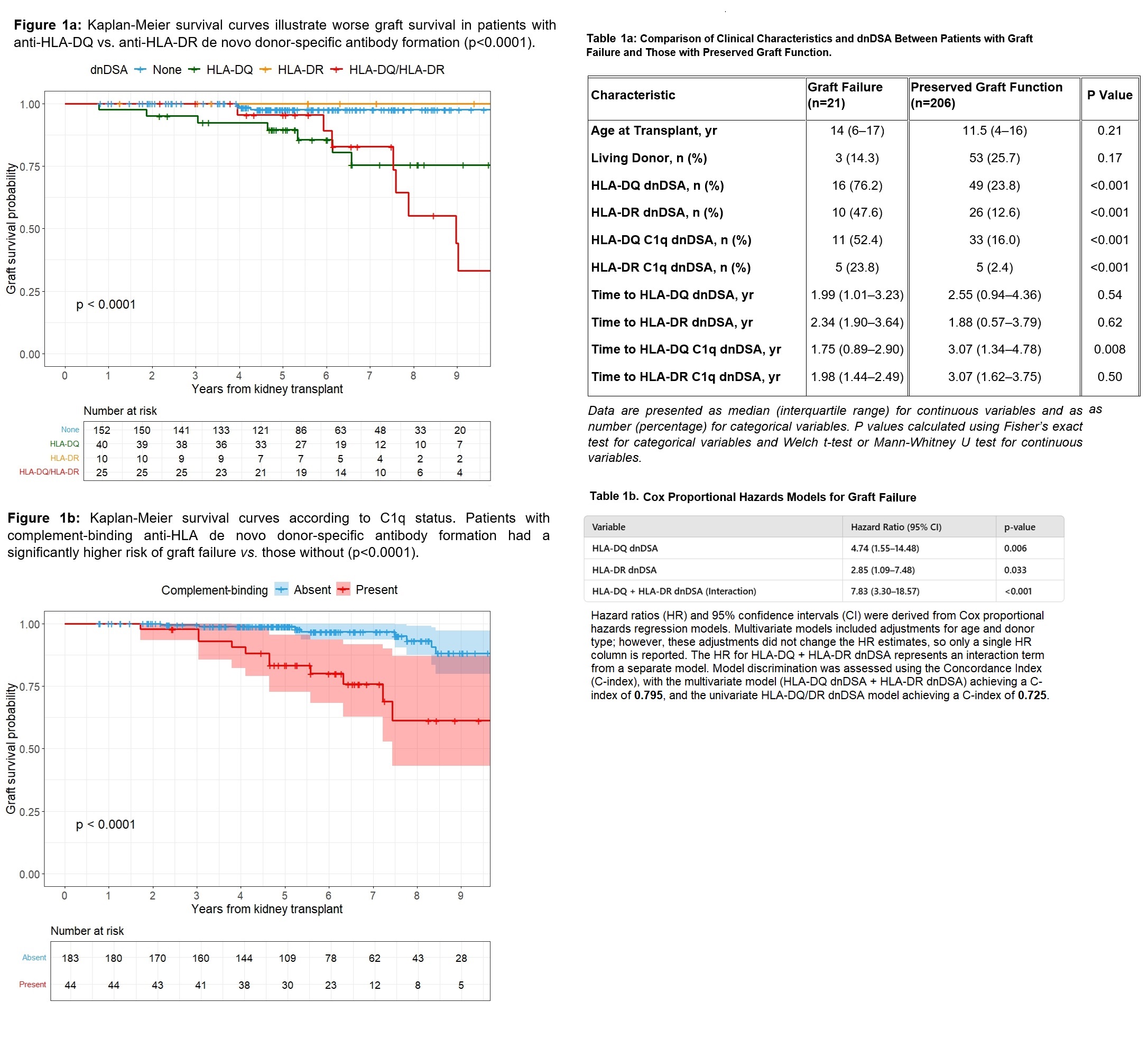
Conclusions: HLA-DQ dnDSA is the dominant driver of graft failure in pediatric kidney transplantation, with a disproportionate impact compared to HLA-DR. The interplay of HLA-DQ and HLA-DR dnDSAs suggests a synergistic effect. Existing risk models do not adequately account for the disproportionate impact of HLA-DQ mismatches. These findings highlight the need for refined allocation strategies and enhanced post-transplant monitoring to mitigate long-term allograft injury.
References:
[1] Rejection
[2] Kidney Transplantation
[3] Immunosuppression
[4] Donor-recipient matching
[5] DSA (Donor-Specific Antibodies)
[6] High-resolution typing
Lectures by Daniel Turudic
| When | Session | Talk Title | Room |
|---|---|---|---|
|
Thu-18 16:00 - 17:00 |
Best Kidney Abstracts | HLA-DQ: The dominant driver of de novo donor-specific antibody-mediated graft failure in pediatric kidney transplantation | MOA 6 |
